The healthcare industry is seeing new trends year on year. Medical billing is gaining centralized attention. We are already in 2026, so understanding the latest medical billing trends is essential for staying competitive and efficient. The global medical billing outsourcing market is forecasted to grow from USD 15.61 billion to USD 40.43 billion by 2033. This CAGR 12.65% growth highlights how strongly healthcare organizations are rethinking their billing strategies
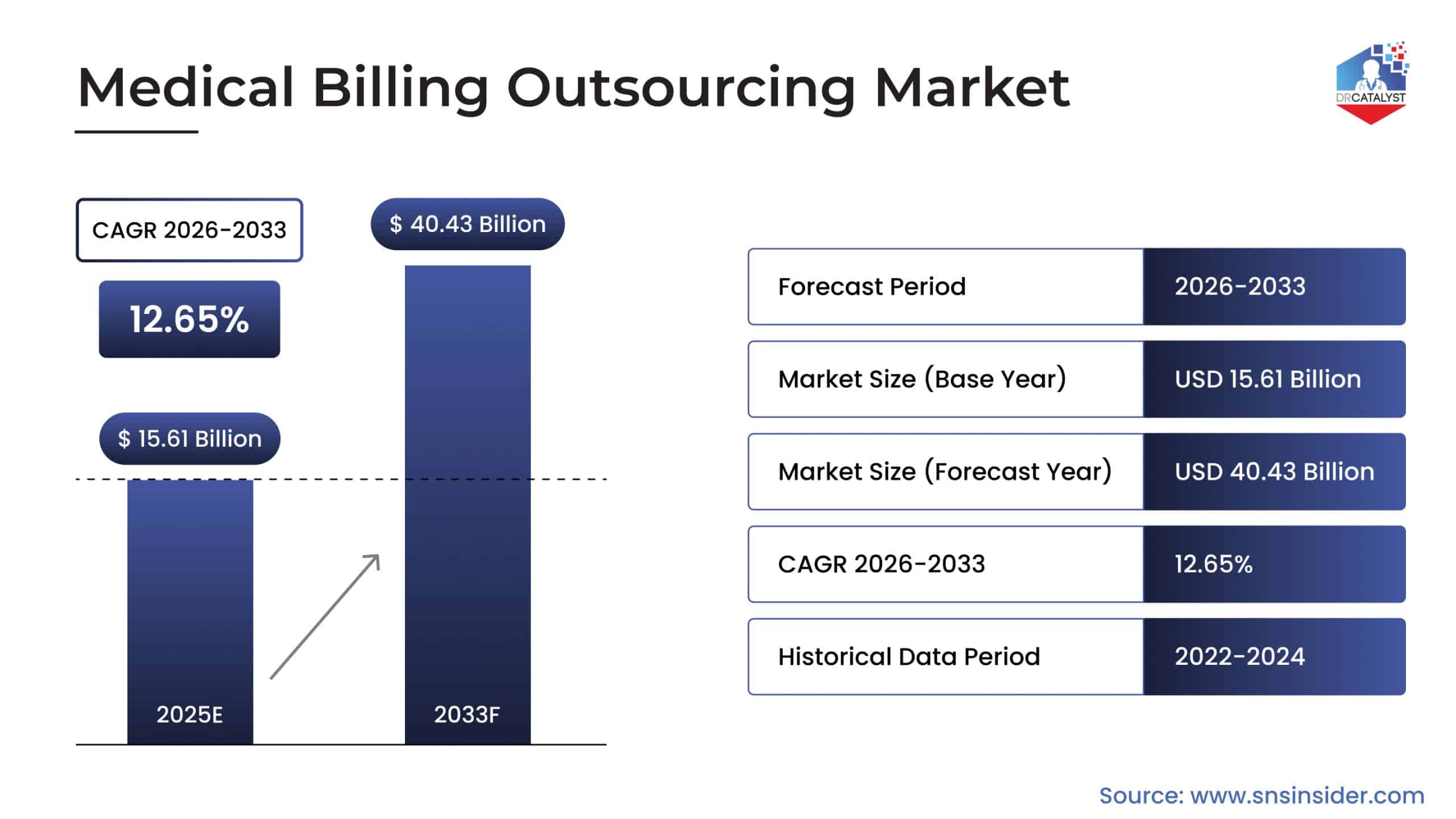
In our experience, whether a small practice or a large healthcare organization, keeping up with healthcare billing trends can make a measurable difference in the revenue flow. Fortune Business Insights show that front-end billing services alone account for nearly 43.8% of outsourced billing demand, underscoring the growing focus on accuracy from the very start of the medical billing process. Let’s explore what’s reshaping the medical billing landscape in 2026.
New Billing Approaches in Value-based Care Models
We have witnessed firsthand that a lot of practices are already switching fee-for-service to value-based care. When you change fee-for-service with value- based care, it fundamentally changes how healthcare gets paid. Healthcare billing trends now emphasize outcome tracking, quality metrics, and bundled payments rather than simple procedure codes. It looks simple but it is tricky. As this requires billing systems to:
Track patient outcomes alongside financial data
Calculate risk-adjusted payments accurately
Coordinate between multiple providers for bundled services
Report quality measures for incentive programs
Understand the differences in medical billing vs. revenue cycle management [Differences in Medical Billing vs RCM for Healthcare Organizations]
Real-Time Claim Adjudication
It is a thing of the past when providers used to wait for weeks to see when whether a claim was accepted or denied. Nowadays, real-time claim adjudication allows providers to know whether a claim will be paid, how much, and if patient responsibility exists. This technology enables front-desk staff to collect accurate patient information before patients leave, dramatically reducing bad debt and improving cash flow. It’s one of the most impactful medical billing trends 2026 is bringing to smaller practices.
Read More: [How to Avoid Common Medical Billing Mistakes]
Telehealth Billing and Remote Patient Monitoring
Telehealth is a permanent part of care delivery. We are seeing an increase in virtual visits and expansion in Remote Patient Monitoring (RPM) programs. To support it, medical billing trends in 2026 now include navigating payer rules for virtual care, time-based billing, and device data reporting. Billing for telehealth and RPM requires:
Accurate use of telehealth-specific CPT and modifier codes
Proper documentation of virtual encounter time and clinical interaction
Ongoing monitoring of payer-specific coverage policies
It sounds simple, but in reality, with frequent regulatory updates and payer variability, even small billing errors in telehealth claims can lead to denials or delayed payments. Practices that fail to adapt risk losing revenue from one of the fastest-growing care models.
Explore how DrCatalyst’s Remote Medical Billers prevent revenue loss for healthcare organizations.
Specialized Billing
As billing becomes more complex with new medical billing trends. In 2026, the need for specialized expertise has never been greater. Different specialties face unique billing challenges, from prior authorization requirements in cardiology to modifier-heavy coding in orthopedics.
Many practices are discovering that generalist billing knowledge isn’t enough anymore. Specialty-specific billing expertise can increase clean claim rates significantly, which directly impacts the bottom line.
AI and Automation with Human Expertise
Artificial intelligence and automation are reshaping healthcare billing trends by improving speed and efficiency. AI-powered tools can assist with charge capture, eligibility checks, and claim scrubbing, helping reduce manual workload and turnaround time. However, AI cannot correct contextual or clinical errors in claim submission. It cannot interpret incomplete documentation, resolve complex denial reasons, or make judgment calls on coding nuances.
This is why AI alone is not enough. The most effective approach in 2026 is AI + experienced billing professionals, where automation handles repetitive tasks and trained staff:
Review flagged claims before submission
Investigate the root causes of denial
Apply payer-specific appeal strategies
This hybrid model ensures accuracy, compliance, and revenue protection.
The Staffing Challenge and Remote Solution
Finding skilled medical billers remains one of the biggest challenges faced by healthcare organizations. High turnover rates and the specialized knowledge requirement make this an ongoing concern. This has accelerated interest in remote billing solutions, with many practices discovering the cost of in-house vs virtual medical billing. Virtual billing teams have access to specialized knowledge without geographic limitations. Additionally, these remote services are offered at a lower cost than maintaining full in-house departments.
Learn more about: [What is better between in-house and Virtual Medical Billing]
Enhanced Data Security and Compliance
With cyber threats getting more sophisticated, billing systems are incorporating advanced security measures. Multi-factor authentication, encrypted data transmission, and regular security audits are becoming standard practice. The medical billing process now includes multiple security checkpoints to protect sensitive patient financial information. Practices that prioritize security build stronger patient trust and avoid costly breaches.
While AI and automation improve efficiency, they also introduce new risks in healthcare billing trends, especially around data security. AI-driven platforms process large volumes of sensitive patient and financial data. This information is a magnet for cyberattacks. Without proper data security, compliance checks, and safeguards, practices face:
Increased risk of data breaches
Potential HIPAA violations
Financial penalties and reputational damage
As a result, security-first billing workflows combined with encrypted systems, controlled access, and human oversight are becoming essential. Technology must enhance billing operations without compromising patient data or compliance.
Read about our commitment to Data Security
Skilled Prior Authorization Management
Prior authorizations have become one of the most time-consuming aspects of medical billing. With more procedures requiring pre-approval, practices are dedicating significant resources to managing the complete process. We’ve seen practices that follow medical billing trends by implementing dedicated prior authorization workflows, tracking approval timelines closely, and maintaining documentation systems. Getting ahead of prior authorizations prevents claim denials and keeps revenue flowing smoothly.
[Explore how DrCatalyst steps forward in Prior Authorization]
Active Denial Management
Healthcare billing trends 2026 are beneficial to healthcare organizations that take proactive approach to claim denials instead of a reactive approach. This means analyzing denial patterns, identifying root causes, and implementing preventive measures. This requires ongoing staff training, regular process reviews, and close attention to payer policy updates.
[Listen how we saved $250,000 under 90 days in denied claims]

How DrCatalyst helps you Navigate Medical Billing Trends in 2026
At DrCatalyst, we make the billing trends possible for your practice. As billing grows more complex in 2026, practices need more than software or generic billing staffing. They need experienced professionals who understand payer behavior, specialty nuances, and the full revenue cycle. Our team provides end-to-end medical billing and revenue cycle management services powered by remote billers.
DrCatalyst works as an extension of your practice, handling everything from charge entry and claim submission to denial management, prior authorizations, and payment posting.
What sets DrCatalyst apart is our human-led, tech-enabled approach:
Skilled billers who understand specialty-specific billing rules and payer policies
Proactive denial prevention through claim audits and root-cause analysis
Dedicated professionals for value-based care billing, telehealth, and RPM services
Secure, HIPAA-compliant workflows with strict data protection standards
Flexible engagement models, whether you need to hire medical billers, augment your team, or fully outsource your revenue cycle management.
While AI and automation help speed up processes, revenue protection still depends on expertise, judgment, and accountability. This is why at DrCatalyst, we combine the efficiency of easily integrating into your EHR with hands-on human oversight to ensure accuracy, compliance, and consistent cash flow. Medical billing trends in 2026 demand greater precision and adaptability. We can help practices reduce administrative burden by successfully processing 40K+ monthly prior authorization tasks to improve clean claim rates and focus on patient care.
Our remote staff work in the protocols of the practice within their business hours. These comprehensive medical billing services are a combination of experienced professionals who understand both the clinical and financial sides of healthcare. Whether you need to hire medical billers to supplement your team or completely outsource your revenue cycle management, we provide solutions tailored to your organization’s unique needs. Our team stays current with the latest trends in medical billing 2026 to ensure your practice maximizes revenue while minimizing administrative burden.
Looking Ahead
The medical billing trends in 2026 shifts toward an increasingly integrated, compliance-focused, and patient-centric approach. As a result, the role of billing has evolved far beyond simply submitting claims and collecting payments. Today, success requires navigating complex reimbursement models, managing high-volume prior authorizations, and maintaining strict compliance within a highly regulated environment. Practices that embrace these transformations while maintaining expert attention to detail will not only thrive but turn these industry challenges into a distinct competitive advantage.
The question for healthcare leaders is no longer whether to adapt, but how quickly they can implement these strategies to protect their practice’s financial future. By joining forces with experienced billing professionals like DrCatalyst, your organization can maximize revenue and turn evolving market trends into long-term financial health.
Contact us today to discover how DrCatalyst can benefit your practice to maximize revenue.