The healthcare landscape is evolving very rapidly. Now, the practices are under more pressure than ever to improve collections, reduce denials, and maintain smooth financial operations. Recent research highlights that effective Revenue Cycle Management (RCM) plays a critical role beyond reimbursement. It directly improves cash flow, operational efficiency, and patient experience in modern healthcare practices. However, it is observed that two terms are often used interchangeably in many communications: Medical Billing and Revenue Cycle Management (RCM).
While they sound similar, they play very different roles in your financial performance. Understanding the distinction can help you identify where your practice needs support services and how the right partner, like DrCatalyst, can help you strengthen your entire revenue ecosystem.
Medical Billing and RCM are crucial for ensuring a practice gets paid for the services it renders. More than 41% of providers reported denial rates above 10% in 2025. This puts unprecedented financial pressure on healthcare practices and exposing weaknesses in revenue workflows. Many organizations mistakenly believe their medical billing is more than sufficient. But, mistaking one for the other can lead to a fragmented financial strategy, resulting in lost revenue, delayed payments, and decreased profitability.
This blog will clarify each concept, highlight why the distinction matters, and help you determine the right approach for your healthcare organization’s success.
What is Medical Billing?
Medical billing is a critical component within the healthcare financial process. It involves converting healthcare services into billing claims and submitting them to payers for reimbursement.
A medical billing team handles tasks like:
- Verifying patient insurance eligibility
- Coding medical procedures and diagnoses
- Creating and submitting claims
- Following up on denials or rejections
- Posting payments and reconciling accounts
Medical billing primarily operates as a reactive, task-focused function. The primary goal is to ensure providers get paid accurately and promptly. It represents just one component of your practice’s overall financial ecosystem. The focus remains narrow, centered on coding accuracy, timely submissions, and pursuing payment for services already rendered.
What is Revenue Cycle Management (RCM)?
If medical billing is the engine, RCM is the entire vehicle, complete with navigation, maintenance, and fuel systems.
Revenue Cycle Management is the end-to-end financial process. It begins the moment a patient schedules an appointment and ends when the balance is fully collected. RCM is a proactive, strategic framework designed to optimize every interaction that affects a practice’s financial outcome. When you hear the phrase medical billing and revenue cycle management used together, remember that medical billing is merely one component of the broader RCM strategy.
RCM covers the full journey:
- Patient registration & insurance verification
- Eligibility checks
- Prior authorizations
- Coding & billing
- Claim submission
- Denial management
- A/R follow-ups
- Patient collections
- Reporting & analytics
- Continuous Optimization
Unlike standalone billing, RCM is a continuous, strategic process designed to reduce revenue leakage. The aim is to improve cash flow and elevate the financial health of the entire practice.
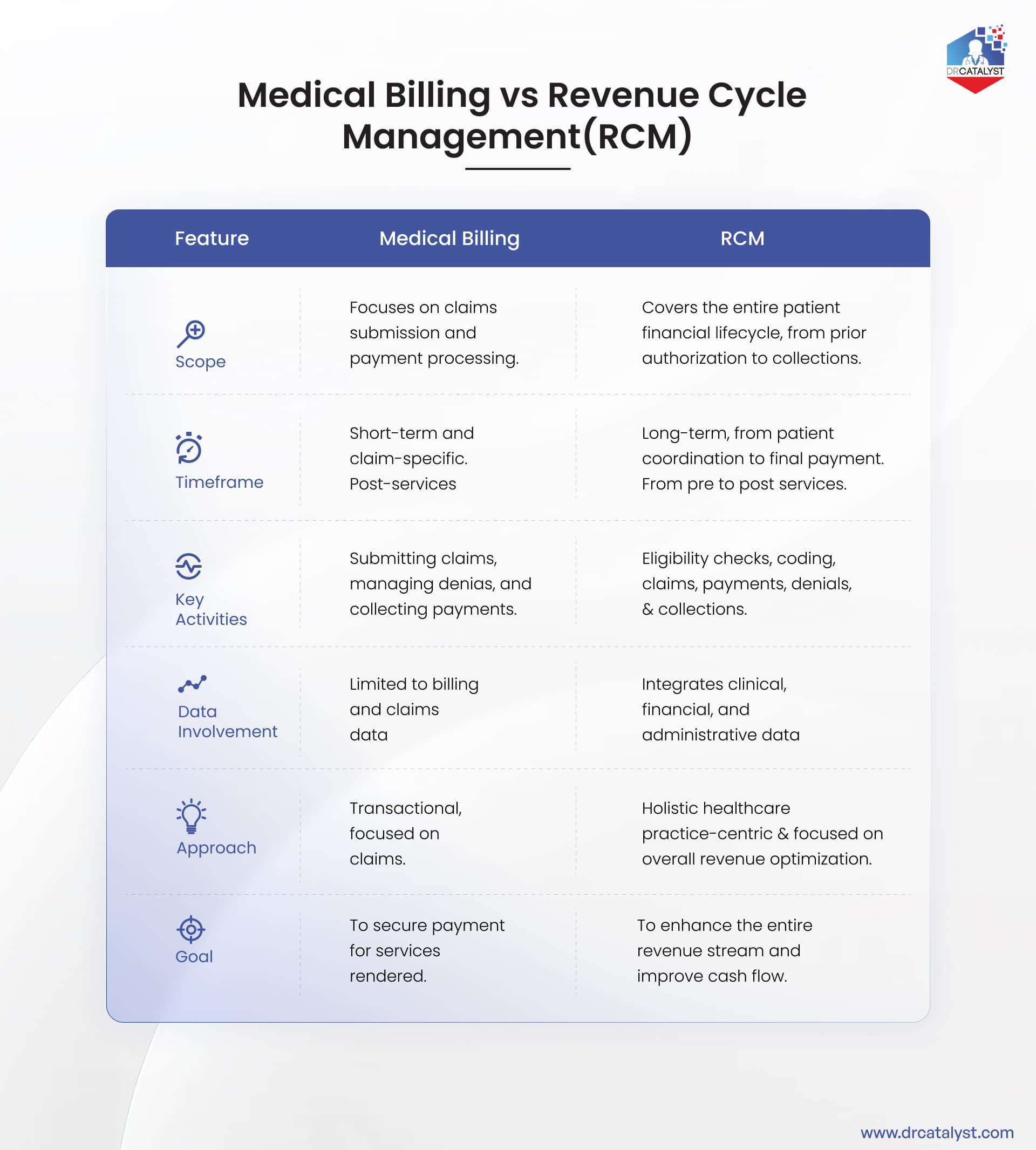
The Difference Between Medical Billing and Revenue Cycle Management
Here’s how medical billing is a key component of the revenue cycle and only one piece of the larger financial picture.
Considering a virtual team to handle these complex processes? Discover the benefits of remote staffing that works like an extension of your team.
Why Understanding the Difference Matters
A practice that relies solely on medical billing services might successfully submit claims but repeatedly face denials for the same reasons. They may be missing prior authorizations or eligibility issues. Often, after services are rendered, these issues are discovered.
As per HFMA, organizations with systematic RCM operations reduce AR days by 20-30%. An RCM approach would identify these patterns, implement front-end verification processes, and prevent the denials from occurring in the first place.
Choosing between Medical Billing and Revenue Cycle Management Services
So which approach does your practice need? The answer depends on several factors:
Consider Medical Billing Services if:
- Your practice has lower claim volume (typically under 200-300 claims per month)
- You have straightforward billing processes with few specialties
- Your denial rates are relatively low
- You primarily need help with coding accuracy and timely claim submission
- Your team can handle front-end processes like registration and eligibility verification
- You’re looking for a cost-effective solution for basic billing operations
Consider Revenue Cycle Management if:
- You have high claim volume or multiple providers
- Your practice includes complex specialties (allergy, behavioral health, FQHC’s)
- You’re experiencing high denial rates or inconsistent cash flow
- You need comprehensive financial analytics and reporting
- You want to optimize patient payment collection processes
- You’re planning to scale or expand your practice
- You need integrated services that connect with your EHR system
- You want proactive denial prevention rather than reactive appeals
Many healthcare practices start with medical billing services and transition to comprehensive RCM as they grow. This evolution is natural as increased complexity demands more sophisticated financial management.
Read More: In-house vs Remote Medical Billing
Why Organizations choose DrCatalyst for Billing & RCM?
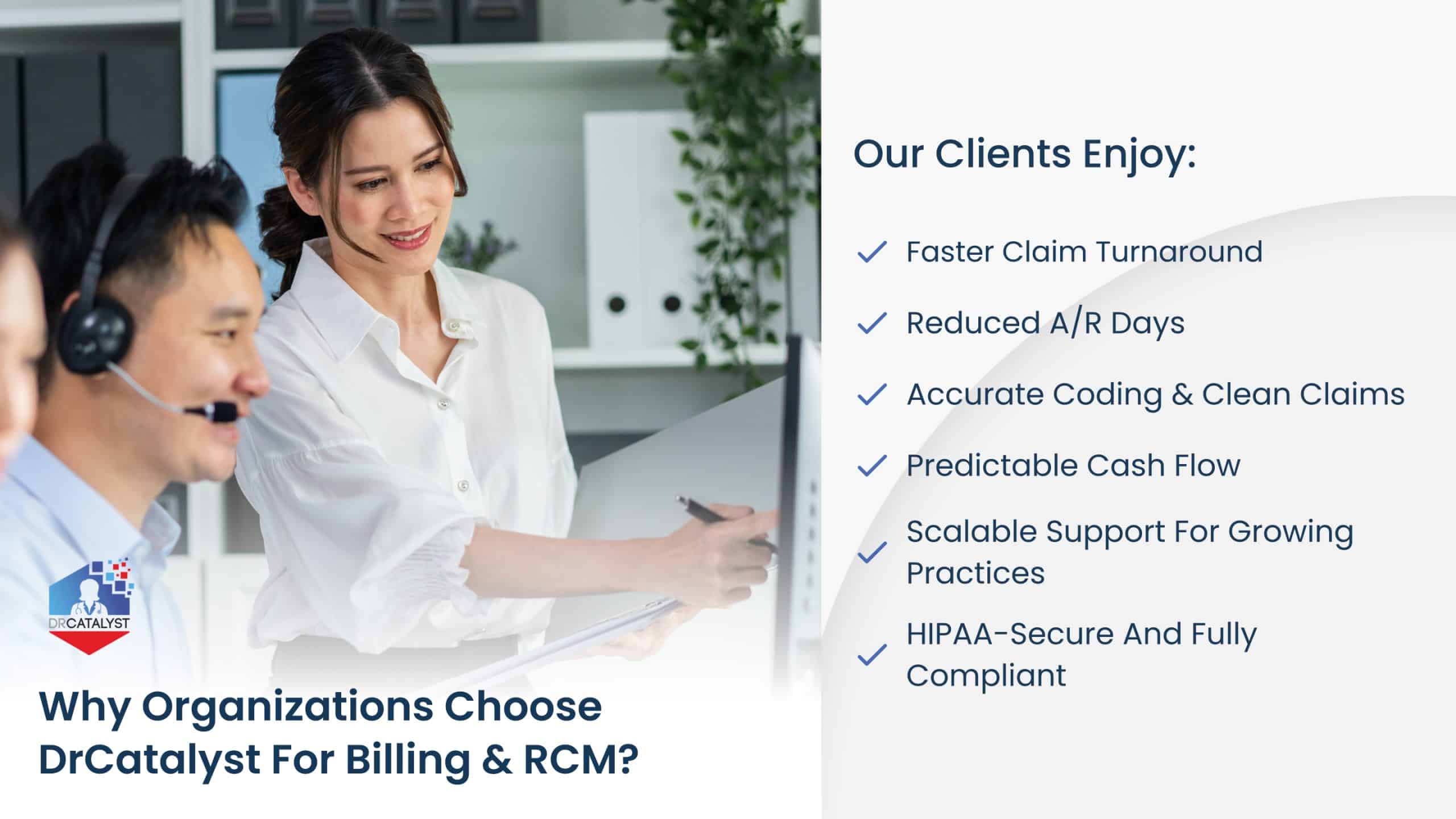
At DrCatalyst, we help healthcare organizations eliminate hurdles, reduce denials, and accelerate collections through 100% dedicated remote teams. Our purpose isn’t just to submit your claims. It is to enhance your organization’s financial well-being by ensuring that every dollar you earn is recovered quickly and efficiently. Whether you’re looking for standalone medical billing support or end-to-end RCM, we tailor our services to your workflow and specialty.
Our clients enjoy:
- Faster claim turnaround
- Reduced A/R days
- Accurate coding & clean claims
- Predictable cash flow
- Scalable support for growing practices
- HIPAA-secure and fully compliant
Our staffing model ensures you get skilled virtual billers, coders, and RCM specialists without the overhead of hiring or training.
Strengthen your Revenue Cycle?
Conclusion
Understanding the difference between medical billing and revenue cycle management helps practices make informed decisions about how to manage revenue operations efficiently. While medical billing ensures immediate claim success, RCM drives overall growth by improving processes, compliance, and cash flow sustainability.
Whether you’re a clinic, hospital, or healthcare group, combining both approaches with a trusted partner like DrCatalyst can transform your administrative performance and unlock smoother, faster reimbursements. Schedule a Consultation to see how we can navigate your billing and RCM strategy for 2026 and beyond.