Prior authorization is a crucial step in healthcare, one that often comes with confusion and frustration for both patients and providers. It’s a required step by insurance companies for many aspects of healthcare, including certain treatments, procedures, and prescriptions. Yet, this also means extra paperwork for your practice. If your practice starts to get overwhelmed, patients are left with longer wait times and, worse, delayed care.
Yet, managing prior authorizations doesn’t have to be this tedious when you have the right approach and staff. With DrCatalyst, you get a helping hand from experienced prior authorization specialists who handle the legwork and ease the administrative load.
Let Our Team Support Yours
What Is Prior Authorization?
Prior authorization (PA), also known as pre-authorization or pre-certification, is a process in which a healthcare provider must get approval from a patient’s insurance company before delivering certain services, medication, or procedures.
Most of the time, it’s insurance companies who require PA, especially:
- Commercial payers
- Medicare Advantage plans
- Some Medicaid plans
Each insurance company has its own list of services that require prior approval, and unfortunately, they are not always the same. The standard services that usually need approval are:
- High-cost procedures (MRI or CT scans)
- Specialized surgeries
- Brand-name or specialty medications
- Ongoing treatments (like physical therapy or injections)
When Does It Happen?
Prior authorization must be acquired before the service is provided. If PA isn’t submitted or gets denied, coverage may be refused, leaving the patient to foot the bill out of pocket. In some cases, if the clinic fails to obtain the required approval, it is unable to bill the patient and ends up absorbing the cost.
How Does Prior Authorization Work?
The importance of prior authorization solutions may not be immediately obvious, but it helps keep critical areas in check.
Cost Control
Healthcare is expensive, and costs continue to rise every year. Insurance companies use prior authorizations to:
- Make sure treatments are medically necessary.
- Prevent unnecessary tests, duplicate services, or overprescribing.
- Help reduce healthcare waste and overspending by ensuring the appropriate use of resources.
Utilization Management
Prior authorization is also a management tool guiding treatment decisions based on:
- Evidence-based medicine.
- Best practices.
- Clinical guidelines.
Preventing Fraud and Overuse
Some medications and procedures have high costs and a high risk of misuse. Prior authorizations prevent fraud and overuse by:
- Catching red flags early.
- Avoiding unnecessary or repetitive care.
- Reducing the chances of fraudulent claims.
Prior Authorization Challenges
Yes, PAs play a crucial role in ensuring the quality and effectiveness of treatments for patients. Yet the process also presents challenges and obstacles that can affect operations and patient care, including:
Administrative Burden
Handling prior authorizations involves:
- Filling out forms.
- Making phone calls.
- Following up with faxes or portals.
For providers and staff, it takes valuable time away from patient care. That’s why some practices dedicate entire teams to managing authorizations.
Delays in Care
When authorizations don’t come through quickly, treatment gets delayed. The consequences can be detrimental to patient outcomes due to:
- Patients waiting for days (or even weeks) for needed care.
- Slower diagnoses.
- Interrupted treatment plans.
These delays can cause frustration for patients and providers alike.
Lack of Transparency
Every insurance company has its own rules, forms, and timelines, and they don’t always make them easy to find, which means:
- Staff are left guessing what’s required.
- Requirements often change without warning.
- Communication can feel disjointed.
If the process is confusing, inconsistent, and unpredictable, that means more delays and unnecessary steps.
Denials and Appeals
Common reasons for denied authorizations are usually because of:
- Late filing.
- Missing documentation.
- Errors (even the most minor ones can cause a denial).
This leads to increased paperwork, appeals, and resubmissions, as well as delayed reimbursements or lost revenue.
How Providers Can Speed Up Prior Authorizations
Prior authorizations don’t have to bring your workflow to a grinding halt. With the right strategies, practices can take control of the process and reduce the burden.
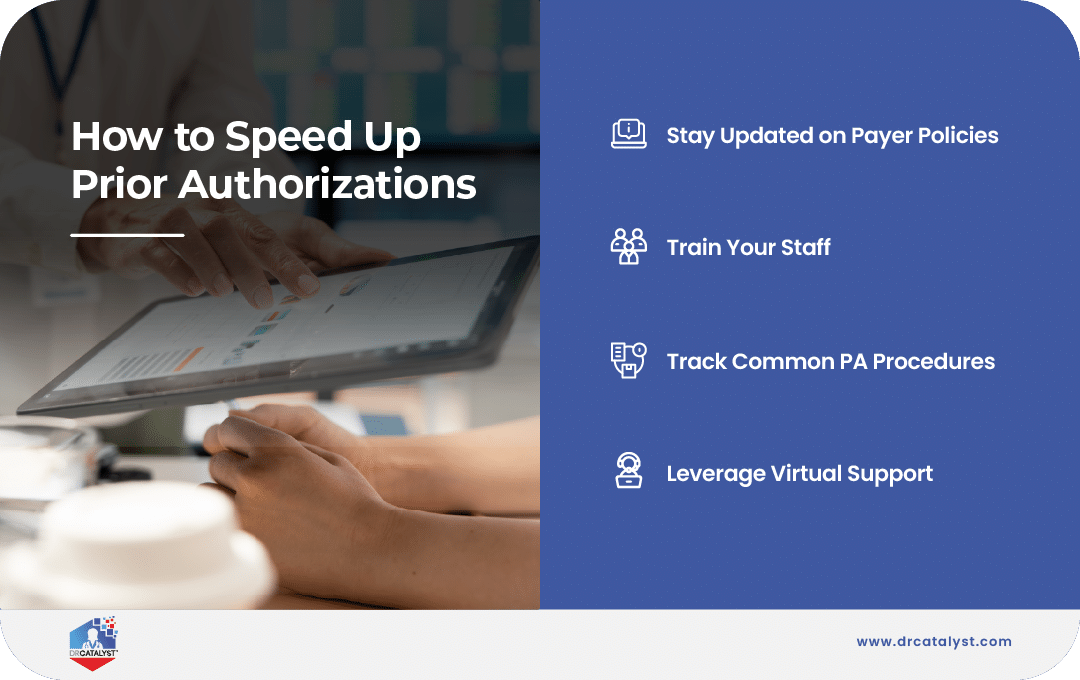
Best Practices That Make a Difference
A few smart moves can go a long way in cutting down delays and denials:
Stay Updated on Payer Policies
Insurance requirements can change quickly. Make sure your team:
- Keeps an updated list of payer-specific PA requirements.
- Subscribes to payer newsletters or bulletins.
- Monitors frequent changes to covered services.
Train Your Staff
Ensure your team knows:
- What documentation each request needs.
- Who to contact at each insurance company.
- How to track and follow up efficiently.
- The patient’s insurance benefits for the service.
Track Common Procedures That Require PA
Chances are, your practice sees repeat requests for:
- Imaging (like MRIs and CTs).
- Certain prescriptions.
- Outpatient procedures.
Don’t Forget About Virtual Support
Many clinics now rely on virtual assistants or remote teams trained specifically to handle prior authorizations. On your behalf, these teams can:
- Check on the patient’s benefits to determine if a PA is required
- Communicate directly with payers and submit requests.
- Stay current on active PA requests and timelines.
- Complete Oversee the full PA process, including appeals if needed.
With the right virtual support, you can lift the burden off your staff and keep operations running smoothly, even during busy seasons.
Lift the Burden of Prior Authorizations with DrCatalyst

Between keeping up with ever-changing payer rules, training staff, and juggling daily volume, many practices find themselves asking: Is there a better way to handle all of this?
There is—and it starts with teaming up with a partner who truly understands your workflow.
With experience dating back to 2010, DrCatalyst serves over 2,300 providers and processes more than 40,000 prior authorization tasks each month–bringing clarity, speed, and peace of mind to an otherwise frustrating process. Our medical billing services don’t just complete the process; we provide reliable, accurate PA staff who get the job done.
- Dedicated Prior Authorization Specialists
Our trained virtual assistants know the ins and outs of payer requirements. They handle the paperwork, follow up on submissions, complete appeals for denials, and even coordinate peer-to-peer reviews so nothing slips through the cracks.
- Expertise That Fits Right In
We plug into your existing processes—no clunky platforms, no added complexity. Just behind-the-scenes staff that instantly feels like part of your in-house team.
- Faster Approvals, Fewer Setbacks
Because we know the payer landscape, we help prevent billing errors and denied claims—keeping care on track and cash flow steady.
Prior authorizations are always part of the job, but the stress, confusion, and delays don’t have to be. Let DrCatalyst achieve smoother operations, quicker approvals, and fewer errors for your team and patients.
Ready to See the Difference?