Introduction
In today’s intricate healthcare landscape, medical billing remains the crucial yet often confusing cornerstone of revenue and patient satisfaction. Whether you’re working in a clinic, managing a hospital, or overseeing administrative operations, the efficiency of the medical billing process has a direct effect on cash flow, regulatory compliance, and operational success.
At its core, medical billing bridges provider services and payers. This ensures that healthcare services are properly coded, submitted, and paid for while patients get transparency rather than unexpected financial burden. Yet, systemic barriers such as rising claim denials, frequent coding errors, and evolving regulatory mandates have increased administrative costs significantly. According to HFMA (Healthcare Financial Management Association), U.S. hospitals lose up to $262 billion annually from denied claims and admin inefficiencies.
This expanded guide will walk you through the world of healthcare billing, covering its fundamental definition, importance, detailed lifecycle, and common challenges. We will also explore how partnering with a specialized medical billing company like DrCatalyst can offer robust medical billing solutions and enhance patient care as well as the financial health of your practice.
What is Medical Billing?
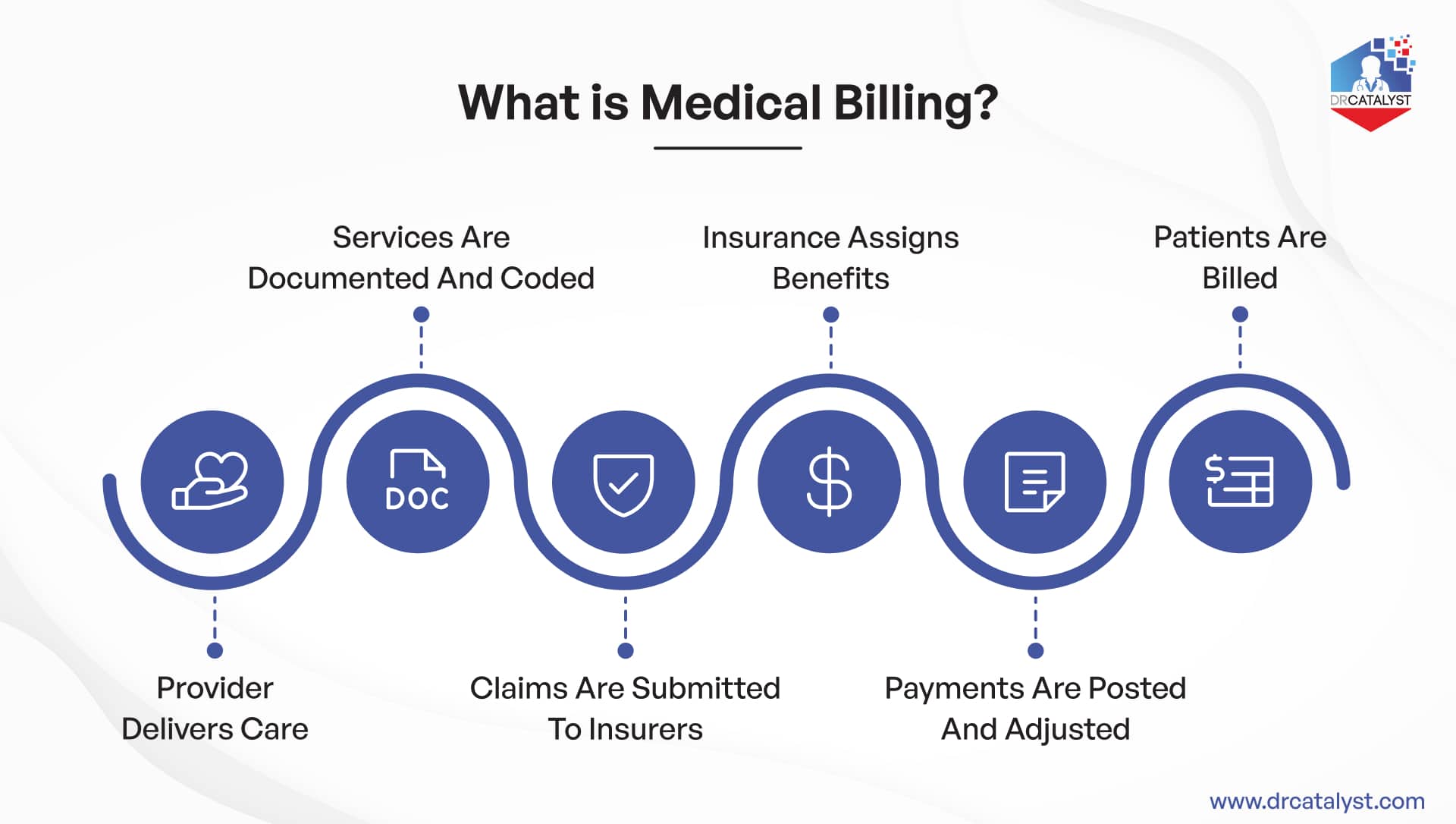
Medical billing in healthcare is the process of translating patient care services into standardized claims submitted to insurance payers for reimbursement. Simply put:
A provider delivers care.
Services are documented and coded.
Claims are submitted to insurers.
Payments and adjustments from insurance are processed.
Patients are billed for any remaining balance.
This process is a critical component of Revenue Cycle Management (RCM) essential for healthcare systems to remain financially stable and patient-focused. Understanding what is medical billing in healthcare is the first step toward optimizing your practice’s financial workflow and ensuring smooth operations.
Types of Medical Billing
Medical billing isn’t a one-size-fits-all practice. Different specialties and healthcare settings often necessitate distinct approaches to billing. Here are some of the common types of medical billing:
- Professional Billing:
This type focuses on the services provided by physicians and other healthcare professionals. It involves coding diagnoses and procedures; submitting claims for consultations, examinations, surgeries, and other direct patient care services. This is typically done using CPT (Current Procedural Terminology) and ICD-10 (International Classification of Diseases, 10th Revision) codes.
- Institutional Billing:
Also known as facility billing, this applies to services rendered by hospitals, clinics, and other healthcare facilities. It covers charges for room and board; equipment usage, nursing care, and other facility-related services. Institutional billing often uses HCPCS (Healthcare Common Procedure Coding System) and revenue codes in addition to ICD-10 codes.
- Hospital Outpatient Prospective Payment System (OPPS) Billing:
This is a specific type of institutional billing for outpatient services provided by hospitals. It operates under a prospective payment system where predetermined rates are paid for specific services, regardless of the actual cost.
- Durable Medical Equipment (DME) Billing:
This involves billing for medical equipment prescribed for use in the home, such as wheelchairs, oxygen tanks, crutches, and continuous glucose monitors. It requires specific codes and documentation to ensure compliance with Medicare and private payer regulations.
- Ancillary Services Billing:
This category includes billing for services that support patient care but are not directly provided by a physician, such as laboratory tests, radiology, physical therapy, and ambulance services.
- Mental Health Billing:
Billing for mental health services often has unique requirements due to the nature of the services and varying insurance coverage for behavioral health. It requires careful coding and documentation to ensure proper reimbursement.
- Chiropractic Billing:
Similar to mental health, chiropractic services have specific billing guidelines, often focusing on spinal adjustments and related therapies.
- Dental Billing:
While distinct from medical billing, dental billing shares many principles, involving claims for dental procedures and treatments.
Each type of billing demands specialized knowledge of coding, regulations, and payer policies to ensure accurate and timely reimbursement.
Benefits of Medical Billing Services
The efficiency of your medical billing system directly impacts your practice’s financial stability and your ability to focus on patient care. Engaging professional medical billing services offers numerous advantages that can significantly boost your revenue cycle management and operational success.
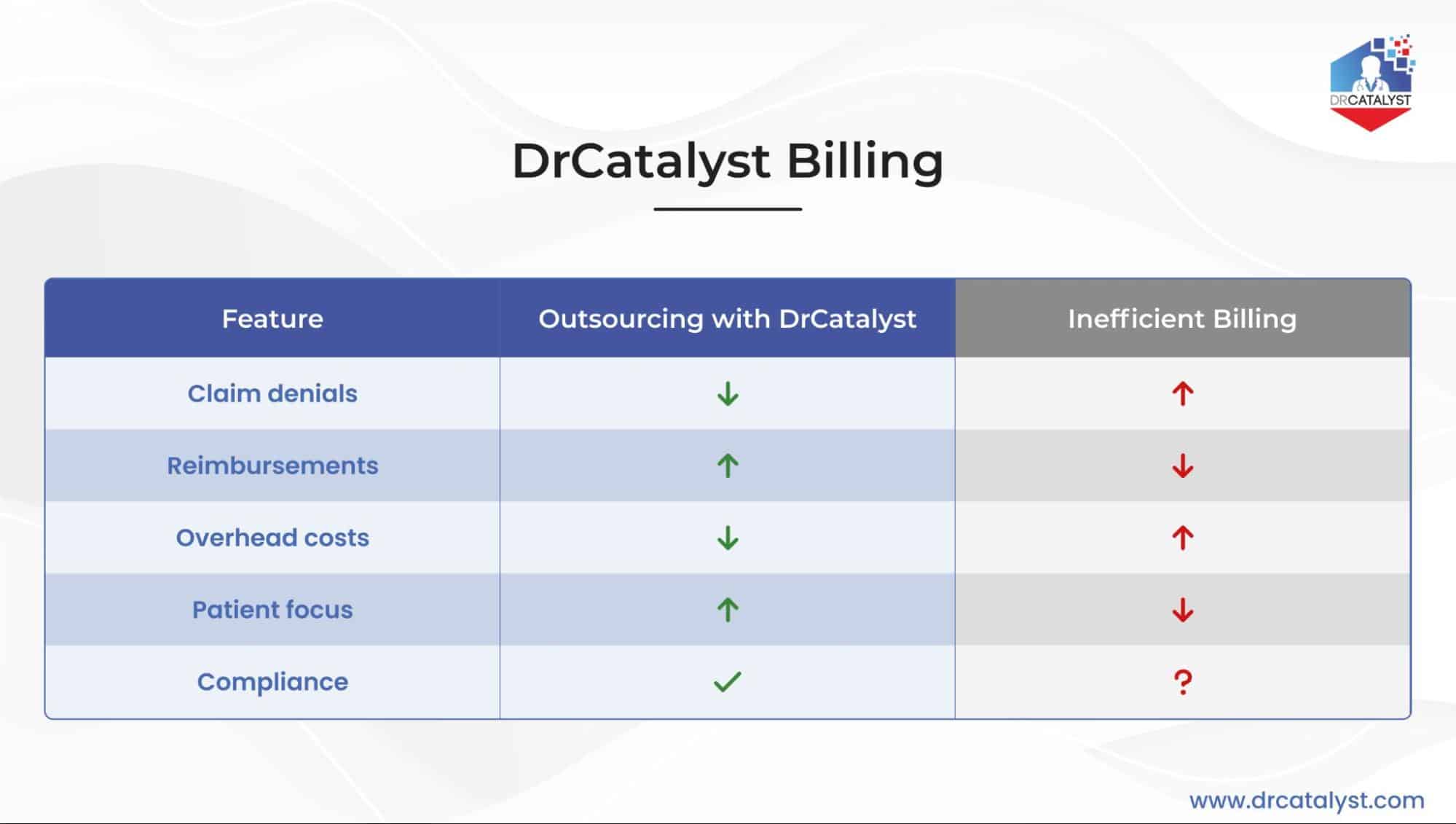
- Reduced Claim Denials:
One of the most significant benefits is a dramatic reduction in claim denials. Professional medical billing companies like Dr Catalyst have proficient billers and coders who are well-versed in the latest coding guidelines (ICD-10, CPT, HCPCS) and payer-specific rules. They meticulously review claims for accuracy, completeness, and medical necessity before submission, significantly lowering the average initial claim denial rate.
- Accelerated Reimbursements and Improved Cash Flow:
With accurate claims and efficient submission processes, payments from insurers are processed much faster. This leads to improved cash flow for your practice, ensuring timely access to funds for operations, staff salaries, and investments.
- Cost Savings:
Medical billing outsourcing can lead to substantial cost savings. Practices can avoid the overhead costs associated with hiring, training, and retaining an in-house billing team, including salaries, benefits, office space, and billing software. Outsourcing can cut billing overhead by up to 30%.
- Enhanced Regulatory Compliance:
The healthcare regulatory landscape is constantly evolving, with new rules and updates to HIPAA, HITECH, and specific payer policies. Medical billing services ensure your practice remains compliant, minimizing the risk of costly audits, penalties, and legal issues.
- Increased Focus on Patient Care:
By offloading the complex and time-consuming task of billing, your administrative staff and providers can dedicate more time and resources to what matters most: delivering high-quality patient care. This improves patient experience and satisfaction.
- Expertise and Specialization:
DrCatalyst with multiple experienced staff members brings an exceptional level of expertise and depth of knowledge. Their services are unmatched against a single onsite biller with limited exposure. The team is better equipped to stay informed about industry changes, denial trends, and evolving billing regulations. They also dedicate sufficient time towards continuous education. This ensures stronger appeal strategies and maximized reimbursement potential.
- Efficient Denial Management:
Even with expert billing, some claims will inevitably be denied. A dedicated medical billing company excels in denial management, promptly identifying the reasons for denial, correcting errors, and resubmitting claims efficiently. This proactive approach helps recover revenue that might otherwise be lost.
- Transparency and Reporting:
Reputable medical billing companies provide detailed reports and analytics on your practice’s financial performance, denial rates, and reimbursement trends. This transparency allows you to monitor your revenue cycle effectively and make informed decisions.
The Medical Billing Lifecycle
The medical billing lifecycle is a systematic process that ensures healthcare providers are reimbursed for the services they deliver. It’s a continuous cycle that, when managed efficiently, underpins the financial health of any healthcare organization. For a more detailed breakdown of each step, you can refer to our blog on the Medical Billing Process.
Here’s a basic overview of the medical billing process:
Patient Registration:
This is the first and crucial step. It involves collecting comprehensive patient demographics, insurance information, and verifying their eligibility and benefits. Accuracy here is paramount, as mistakes in this phase can lead to a significant percentage of claim denials or collecting the due amount from the patients.
Charge Capture & Medical Coding:
Once a patient receives care, the services including procedures, treatments, medications, and supplies are all documented. These are then translated into billable charges through medical coding. They adhere to standardized classification systems such as ICD-10 (for diagnoses), CPT (for procedures), and HCPCS (for equipment and services). Accurate coding ensures both compliance and proper reimbursement.
Claim Submission:
Once services are coded, a clean claim is generated and submitted electronically to the patient’s insurance payer, often through a clearinghouse that reviews claims for errors before forwarding them.
Payment Posting:
When the insurance company processes the claim, they send an Explanation of Benefits (EOB) or Electronic Remittance Advice (ERA) detailing the payment, any adjustments, and reasons for denial. This information is then posted to the patient’s account.
Denial Management:
If a claim is denied, this critical step involves identifying the reason for denial, correcting any errors, and appealing or resubmitting the claim. Effective denial management is crucial for recovering lost revenue.
Patient Billing & Collections:
Best practice dictates that patient financial responsibility should be determined and collected at the point of service, following a comprehensive verification of benefits. Once the insurer has adjudicated the claim, the account is reconciled to reflect any remaining balance. This systematic approach not only strengthens revenue cycle efficiency but also reduces the incidence of delayed or outstanding patient payments.
Each step in the medical billing lifecycle is interconnected, and inefficiencies in one area can cascade into others, affecting overall revenue.
Medical Billing Challenges
Despite its critical importance, medical billing continually faces challenges that can significantly impede cash flow and operational success for healthcare providers. These challenges in medical billing are often complex and multifactorial.
High Claim Denial Rates:
The average initial claim denial rate in the U.S. continues to be a major hurdle. According to the 2025 published report, it rose to 11.81%, reflecting a 2.4% increase year over year. Denials are most often tied to medical necessity and coding errors, patient eligibility issues, and prior authorization requirements. With many experienced billers who stayed with practices for decades now retired, practices are struggling to keep up with the complexity of billing. This makes claim denials an even bigger challenge!
Complex Coding and Regulatory Changes:
Medical coding is constantly evolving with updates to ICD-10, CPT, and HCPCS codes. Staying abreast of these changes, coupled with new payer policies and government regulations (like HIPAA and MACRA), requires continuous education and vigilance. Non-compliance can lead to audits, fines, and revoked licenses.
Prior Authorization Hurdles:
Obtaining prior authorization from insurance companies for certain procedures, medications, or services is a time-consuming and often frustrating process. Delays or denials in prior authorization can disrupt patient care and lead to significant revenue loss.
Staffing Shortages and Training:
Many practices struggle to find and retain qualified medical billers and coders. The complexity of the job requires extensive training, and high turnover rates can severely impact the practice’s financial viability.
Outdated Technology and Manual Processes:
Relying on outdated billing software or manual processes increases the risk of errors, slows down claim submission, and hinders efficient denial management. Integrating disparate systems and ensuring interoperability can also be a significant challenge.
Managing Underpayments and Appeals:
Insurance companies often underpay claims, and identifying these discrepancies requires meticulous review. The appeals process for underpaid or denied claims is complex and time-consuming, requiring detailed documentation and persistence.
Patient Financial Responsibility:
Collecting co-pays, deductibles, and patient balances after insurance payments can be challenging. Patients may be confused by their bills, leading to payment delays or uncollected revenue.
Cybersecurity Threats:
With the increasing digitalization of healthcare data, medical billing systems are vulnerable to cyberattacks. Data breaches can compromise sensitive patient information, leading to severe penalties under HIPAA and erosion of patient trust.
Integration with EHR/EMR Systems:
Direct integration between billing software and Electronic Health Record (EHR) or Electronic Medical Record (EMR) systems is crucial for efficient charge capture and claim generation. Poor integration can lead to data entry errors and workflow bottlenecks.
The Shift to Value-Based Care:
The move from fee-for-service to value-based care models introduces new billing complexities, requiring practices to track outcomes, quality metrics, and patient satisfaction in addition to traditional service codes.
Navigating these challenges requires a robust strategy, skilled professionals, and often, the right technological solutions or external partnerships.
Why is DrCatalyst Your Best Choice for Medical Billing?
Navigating the complexities of medical billing demands more than just processing claims; it requires precision, expertise, and unwavering dedication to compliance. At DrCatalyst, we understand these challenges, which is why we offer comprehensive medical billing services designed to optimize your revenue cycle and alleviate administrative burdens.
As a leading medical billing company, we leverage advanced technology and a team of certified, HIPAA-compliant medical billers and coders. They ensure accurate claim submissions, minimize denials, and accelerate reimbursements. We are not just a service provider; we are an extension of your practice, committed to maximizing your financial health while you focus on delivering exceptional patient care. With DrCatalyst, you gain a partner dedicated to transparency, efficiency, and significant improvements in your practice’s profitability.
Conclusion
Medical billing is undeniably the financial backbone of any healthcare practice. From the initial patient encounter to the final payment, every step in the medical billing lifecycle is crucial for ensuring revenue integrity and operational sustainability. While the process is complex and riddled with challenges from managing escalating claim denials and navigating intricate coding regulations to ensuring robust data security, understanding these nuances is the first step toward effective management.
By embracing an extensive approach that includes accurate coding, efficient claims processing, proactive denial management, and unwavering commitment to compliance, healthcare providers can significantly improve their financial health. Partnering with a specialized medical billing company like DrCatalyst offers a strategic advantage. We provide the expertise, technology, and support needed to maximise your revenue, stabilize your revenue cycle, and reduce administrative overheads. Ultimately, it allows you to dedicate more time and resources to what matters most: delivering outstanding patient care. Investing in a robust medical billing system and reliable medical billing solutions is not just about financial gain; it’s about building a stable, compliant, and patient-focused healthcare practice for the future.
Need Expert Medical Billing Services?
If you’re struggling with rising claim denials, complex coding, or slow reimbursements, let us at DrCatalyst offer you an extra hand. We can make your medical billing process efficient, improve cash flow, and ensure compliance. Our qualified experts are ready to transform your revenue cycle. Beyond medical billing, DrCatalyst offers a range of remote staffing services to optimize your healthcare operations. Discover how our comprehensive solutions can empower your practice.