Beginning January 1, 2026, California will lead the nation with a new law, Senate Bill 729 (SB 729), which mandates that most large-group health insurance plans must cover comprehensive infertility diagnosis and treatment. This includes in vitro fertilization (IVF). This transformative legislation represents a major step forward in reproductive health equity, expanding access for thousands of individuals and couples across the state.
Key Details: What Does SB 729 Provide?
SB 729 requires large, fully insured employer health plans (those with more than 100 employees) to offer fertility coverage, including:
Diagnostic testing and treatment for infertility.
Up to three completed egg retrievals per policy.
Unlimited embryo transfers per medical guidelines.
Coverage for LGBTQIA+ individuals, single parents, and others previously excluded by narrow definitions of infertility.
The law notably broadens the eligibility criteria for coverage, ensuring that reproductive services are accessible to a diverse and inclusive group of Californians.
When Does the Law Take Effect?
The implementation of SB 729 has been officially postponed from July 2025 to January 1, 2026. It allows insurers, clinics, and employers time to adapt to the sweeping changes. Coverage begins for large-group plans renewing on or after that date, while California’s state employees (covered by CalPERS) will see the update in their plans starting July 1, 2027.
Who Will Benefit From Expanded Coverage?
SB 729 is specifically designed to bring fertility treatments within reach for:
Heterosexual couples facing infertility diagnoses.
Same-sex couples and LGBTQIA+ individuals seeking family-building services.
Single parents-to-be.
Cancer patients preserving fertility before treatment.
Employees of covered California-based large-group employers.
Nonetheless, the exceptions remain. The smaller employer plans (with fewer than 100 employees), religious organizations, and self-funded employer health plans aren’t required to comply. Medicare and Medi-Cal (Medicaid) beneficiaries are explicitly excluded from this state mandate. This is because SB 729 only governs fully insured commercial group health plans regulated by the California Department of Insurance (CDI) or the Department of Managed Health Care (DMHC). However, advocacy groups continue to push for broader mandates.
Why This Legislation Is Historic
The average cost of one IVF cycle in California can exceed $12,000, often putting parenthood out of reach for many families. By mandating insurance coverage, SB 729 removes a significant financial barrier and reaffirms that reproductive health is essential. For LGBTQIA+ and single patients, the law’s modernized definition of infertility ensures access without hurdles based on outdated policies.
Dr. Deborah Wachs, a reproductive endocrinologist, calls this law a “milestone in expanding access to fertility care across California,” underscoring its potential to change countless lives.
What Should Patients and Clinics Do Now?
Clinics across California are encouraging patients to begin fertility testing and consultations today. This helps individuals understand their reproductive health now, and allows time to craft a personalized plan aligned with future insurance benefits and changing laws. Fertility specialists, meanwhile, are preparing for an anticipated surge in demand once coverage expands.
Stop by our ASRM booth to discuss how to align your clinic’s operations with the new SB 729 mandate.
How DrCatalyst Can Support Fertility Clinics?
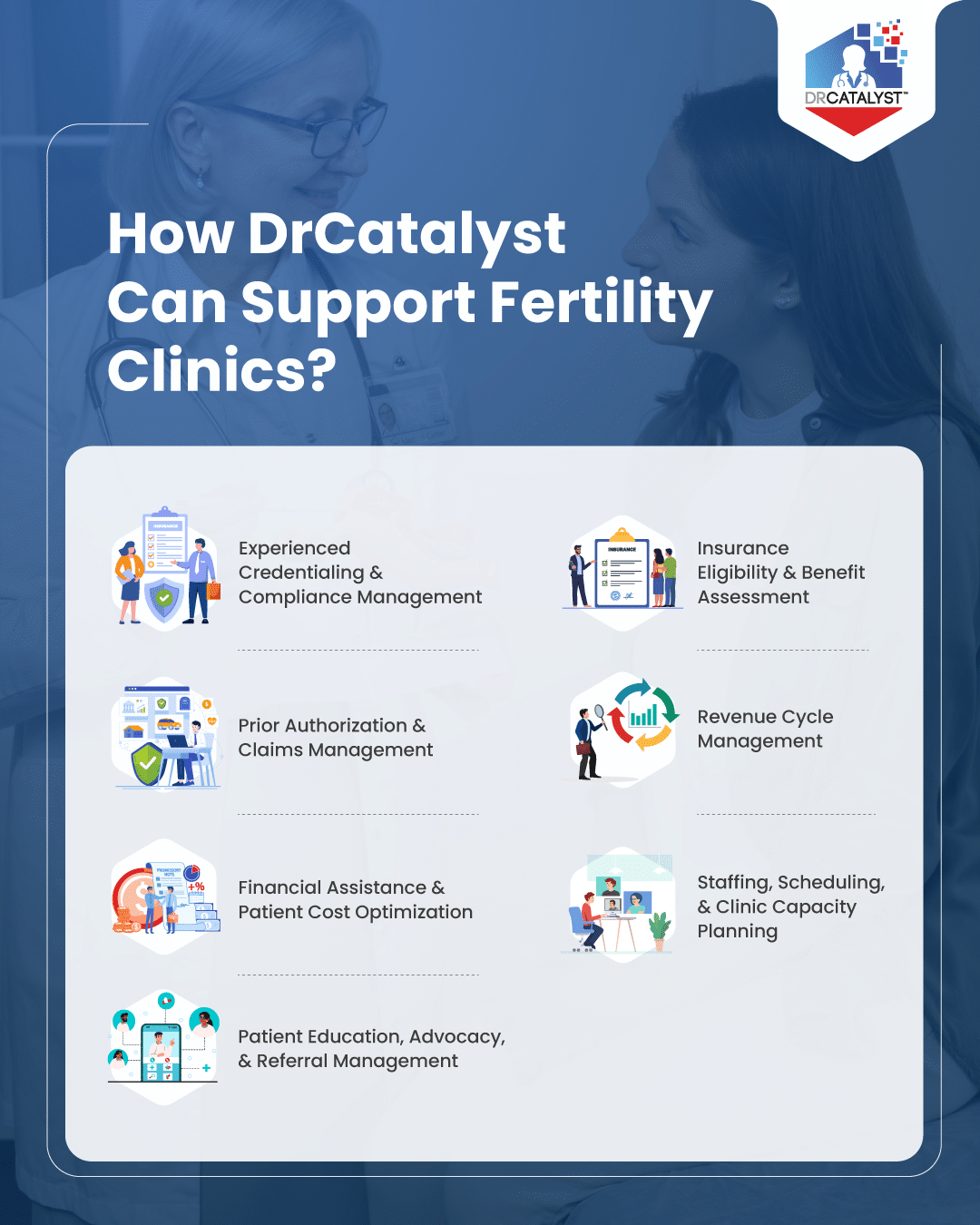
With expanded coverage comes an urgent need for clinics to optimize operations, manage higher patient volumes, and ensure regulatory compliance. It creates a significant need for fertility providers to delegate operational tasks and focus on patient care. DrCatalyst comes to rescue as a comprehensive service platform. Here’s how DrCatalyst helps providers to efficiently utilize their onsite resources –
Experienced Credentialing & Compliance Management
As clinics prepare to expand under SB 729, timely provider credentialing and payer enrollment become essential for uninterrupted operations. In California, this process is often more complex due to the state’s high volume of providers. This can create application backlogs, and the need for meticulous compliance with both state-specific regulations (like the California Department of Public Health) and unique payer requirements, such as those set by large entities like Medi-Cal and specific California-based health plans (e.g., Blue Shield of California). DrCatalyst’s Credentialing Services help physicians and fertility specialists get credentialed quickly with major insurance carriers and smaller IPAs. This minimizes claim denials, shortens reimbursement cycles, and keeps fertility practice compliant and ready to serve new patients under the updated coverage laws.
Schedule a call with us today to discover how DrCatalyst can help you with insurance navigation, end-to-end revenue cycle optimization, and more in this new era of California fertility care.
Insurance Eligibility & Benefit Assessment
DrCatalyst’s virtual eligibility coordinators audit insurance plans, verify SB 729 applicability (fully insured vs. self-insured, renewals, exemptions), and forecast benefit activation so clinics and patients understand coverage timing and minimize financial surprises.
Prior Authorization & Claims Management
Certified staff handle preauthorization paperwork, medical necessity documentation, appeals, coding checks, and help clinics meet insurer compliance requirements for infertility treatments newly covered under California SB 729.
Revenue Cycle Management
DrCatalyst’s end-to-end RCM services include billing, coding, claims submission, follow-up, and payment posting. The aim is to maximize insurance reimbursements for California Senate Bill (SB- 729) covered services and protect fertility clinics’ financial health as demand surges.
Financial Assistance & Patient Cost Optimization
Through robust billing and benefits verification, DrCatalyst helps triage out-of-pocket costs related to fertility medications, non-covered procedures, and co-insurance. They simplify collections and documentation to reduce cost burden for patients and strengthen recoveries for clinics.
Staffing, Scheduling, & Clinic Capacity Planning
DrCatalyst provides remote staffing (medical assistants, phone receptionists, schedulers) and administrative support. This allows clinics to expand operations, manage appointment volume, and maintain smooth workflows as more patients seek care under SB 729.
Patient Education, Advocacy, & Referral Management
DrCatalyst coordinates patient communications, educates about California SB 729 benefits, handles referrals for specialized reproductive services, and advocates on behalf of patients for denied or disputed claims.
Each of these services enables fertility clinics to confidently adapt and thrive under the new California Senate Bill 729 landscape, supporting both operational efficiency and optimal patient outcomes with compliant practices.
Challenges, Critiques & Open Questions
No law is flawless. As SB 729 rolls out, several challenges remain:
Implementation & Oversight Complexity
Translating broad mandates into rules for benefit design, coverage definitions, and dispute resolution is complex. Regulatory agencies must define acceptable limits, appeals processes, and enforcement.
Ambiguities in Third-Party Services
The law provides a framework, but details remain unclear around coverage of donor gametes, embryo storage beyond clinical necessity, gestational surrogacy, lab costs, and other ancillary services.
Coding Accuracy & Denial Challenges
Fertility treatments involve highly specialized procedures such as IVF, egg retrieval, cryopreservation, hormonal therapy, and many more. Each of these procedures require distinct CPT and ICD-10 coding. As SB 729 expands coverage, incorrect or incomplete coding can trigger denials or delayed payments, especially when insurers adopt differing medical necessity criteria. With evolving payer guidelines in California, coding precision, strong documentation, and preauthorization will be vital in reducing rejections, maintaining compliance, and protecting reimbursement timelines.
Cost Inflation & Premium Pressure
Insurers and employers may respond by raising premiums or narrowing networks. Some worry about trade-offs in plan generosity elsewhere to accommodate fertility coverage.
Access & Institutional Capacity
As demand rises, not all clinics will be able to scale quickly. Patients in rural areas or underserved communities may still face obstacles.
Disparities Within the System
Coverage doesn’t equal access. Out-of-pocket costs, travel, time off work, and social determinants of health will still affect who truly benefits.
Resistance from Self-insured Plans & Employers
Because self-insured plans are exempt, some workers may remain uncovered despite the law. Employers may resist adopting voluntary fertility add-ons or passing costs to employees.
Legal & Political Threats
As reproductive health policy remains politically contentious nationwide, future legal or political pushes may target assisted reproductive technology coverage.
However, despite these uncertainties, SB 729 is a transformative step, one that emphasizes fertility care as a right and medical necessity, rather than elective luxury.
What to Expect in 2026 and Beyond?
January 1, 2026 will mark the formal start date for many fully insured group plans to include infertility and IVF benefits. In late 2025, insurers and regulators will issue implementation guidance on benefit design, appeals, and compliance. Clinics will begin seeing increases in new patient volume and demand for advanced reproductive services.
DrCatalyst helps in collecting outcome data to refine protocols and contribute to research and evidence-based fertility practice. The experience of California may influence other states considering similar mandates, especially as fertility policy becomes a national priority. Over time, norms may shift: fertility coverage may become standard in health plans, making family building more accessible nationwide.
Conclusion
California’s SB 729 is a watershed moment in reproductive health policy. By mandating IVF and infertility treatment coverage for many insured Californians, it seeks to break down long-standing financial and structural barriers to family building. The delay to January 2026 gives stakeholders time to prepare, but time is of the essence for patients and providers alike.
For those on a fertility journey, aligning strategy, timing, and insurance will be critical. That is where DrCatalyst’s holistic offering can make a difference. They guide patients through eligibility, insurance navigation, multi-cycle planning, prior authorization, and outcomes management. With SB 729’s promise and DrCatalyst’s support, the path to parenthood may become more achievable.