The landscape of medical billing services has regulatory changes, technological advancements, and shifting reimbursement models. CMS predicts that the provider spending will increase by 50% between 2022 and 2030. Some factors, like rising healthcare costs, shrinking reimbursements, and ongoing staffing shortages, are responsible for an increase in provider spending.
Whether you’re a solo practitioner, a growing multi-provider practice, or a specialized healthcare facility, understanding the true cost of medical billing services can be challenging. In this blog, we will walk you through the key cost drivers, realistic price ranges, hidden fees in medical billing services, and more. At the end, there is DrCatalyst’s transparent approach to help you make informed decisions and get more value from every dollar invested.
Factors that influence Medical Billing Services Cost in 2026
The cost of medical billing services is rarely a one-size-fits-all situation. Some of the variables are behind the bulked-up quote you receive from a vendor:
Practice Size and Provider Count
The size of the practice impacts the pricing of medical billing services. In the case of Solo practitioners, they face different cost structures compared to multi-provider practices or large healthcare groups.
Solo Practices
The recent industry data for solo practices displays an approximate 10-12% of total collections when they outsource medical billing services. If it is calculated, it means that a practice generating $200,000 in annual revenue is roughly paying $20,000- $24,000 in yearly billing costs.
Large Practices
The practices in multi-location or those with 10+ providers often negotiate lower percentage rates (4-7% of collections) due to higher claim volumes and economies of scale.
Types of Specialties
High-complex Specialties
The specialties, such as cardiology, OB-GYN, behavioral health, oncology, neurology, and more, have complex coding, payer variability, and documentation requirements. As a result, cardiology, OB-GYN, behavioral health, and more specialties incur higher healthcare billing costs.
Moderately-complex Specialties
The moderately complex specialties include internal medicine, family practice, and pediatrics. These specialties generally fall into the 5-8% range for outsourced billing services. These specialties have established coding patterns but still require knowledgeable billers familiar with their specific documentation requirements.
Monthly Claim Volume
The practices with high claim volume will benefit from tiered pricing, whereas smaller clinics might pay a higher percentage per claim. The organizations that submit 1,000+ claims monthly can often negotiate rates between 4-7% as they provide a predictable revenue stream to billing companies.
Services included in the Contract
Before you start a medical services contract, ensure you have listed down your requirements. The clarity in terms of a complete Revenue Cycle Management (RCM), from eligibility verification to denial management, or just back-end claim submission in critical. While some billing companies do claim submission well, others may not be proficient at it. The detailed contract with the billing company will list down the included and excluded billing tasks to help the practice better for their future. The breadth of the required services will automatically drive the cost for them.
Pricing Model
The generic service providers in the market typically use a percentage-of-collections model, a per‑claim fee, a per‑provider monthly fee, or hourly/project-based pricing. Each of these pricing models comes with pros and cons for predictability and ROI.
Software Integration
Whether you use your existing EHR or adopt the vendor’s platform can significantly impact the total healthcare billing cost. In absence of an EHR integration, every requirement to switch the billing software can cost you time in the transition with a lack of transparency.
Compliance & Regulatory Overhead
With annual updates to coding (CPT, ICD-10) and FQHC billing-specific PPS rules, services that invest in rigorous compliance expertise help mitigate audit risk, which can be reflected in pricing. Organizations should avoid to partner with vendors who work with outdated codes which causes delayed and lost revenue for them.
Onshore vs Hybrid/Offshore Staffing
It is a well-known fact that the cost of In-house teams is usually higher. But, the hybrid or offshore models can lower the healthcare billing cost while still delivering strong performance when well managed.
Pro Tip : Before signing a contract, ensure you understand the core differences between a billing-only model and a complete RCM approach. Read our guide on [Medical Billing vs RCM].
Cost Comparison for Medical Billing Services in 2026
While specific figures are still evolving, current trends allow for an informed projection. The standard pricing ranges have been listed below:
1. Percentage-Based Model (Most Common)
The Percentage Model includes 5% to 8% of monthly collections. This remains prevalent as it aligns the billing company’s success with your own. While percentage-based pricing may seem expensive, it often delivers higher net revenue due to improved collections and faster reimbursements.
Advantages of Percentage-based Pricing
Aligns billing company incentives with your collection goals
Scales naturally with practice growth
No billing costs if you don’t collect revenue
Predictable expense as a percentage of revenue>/p>
Creates a partnership for mutual success
Eliminates the risk of sufficient, qualified billing staff for the clinic
Disadvantages of Percentage-based Pricing
It can be pricey with growing practice revenue
Less control over total annual costs
May incentivize quantity over quality in some cases
2. Flat Fee per Claim
Trends suggest $3 to $10+ per claim, with complexity being the key determinant. A visit claim costs less than a detailed procedural claim for surgery or behavioral health. In the same way, In-house billing costs: $45,000–$75,000+ annually per biller (salary, benefits, training)
3. Monthly Subscription
Some vendors charge a fixed monthly fee based on the number of providers. This is ideal for budget predictability but may not account for seasonal surges in patient volume.
4. Per-provider monthly fees
Some vendors charge 200–1,000 USD+ per provider per month for bundled practice management and billing support, sometimes tied to volume thresholds.
Looking for help choosing the right vendor beyond just price? Read: Choosing a Medical Billing Company
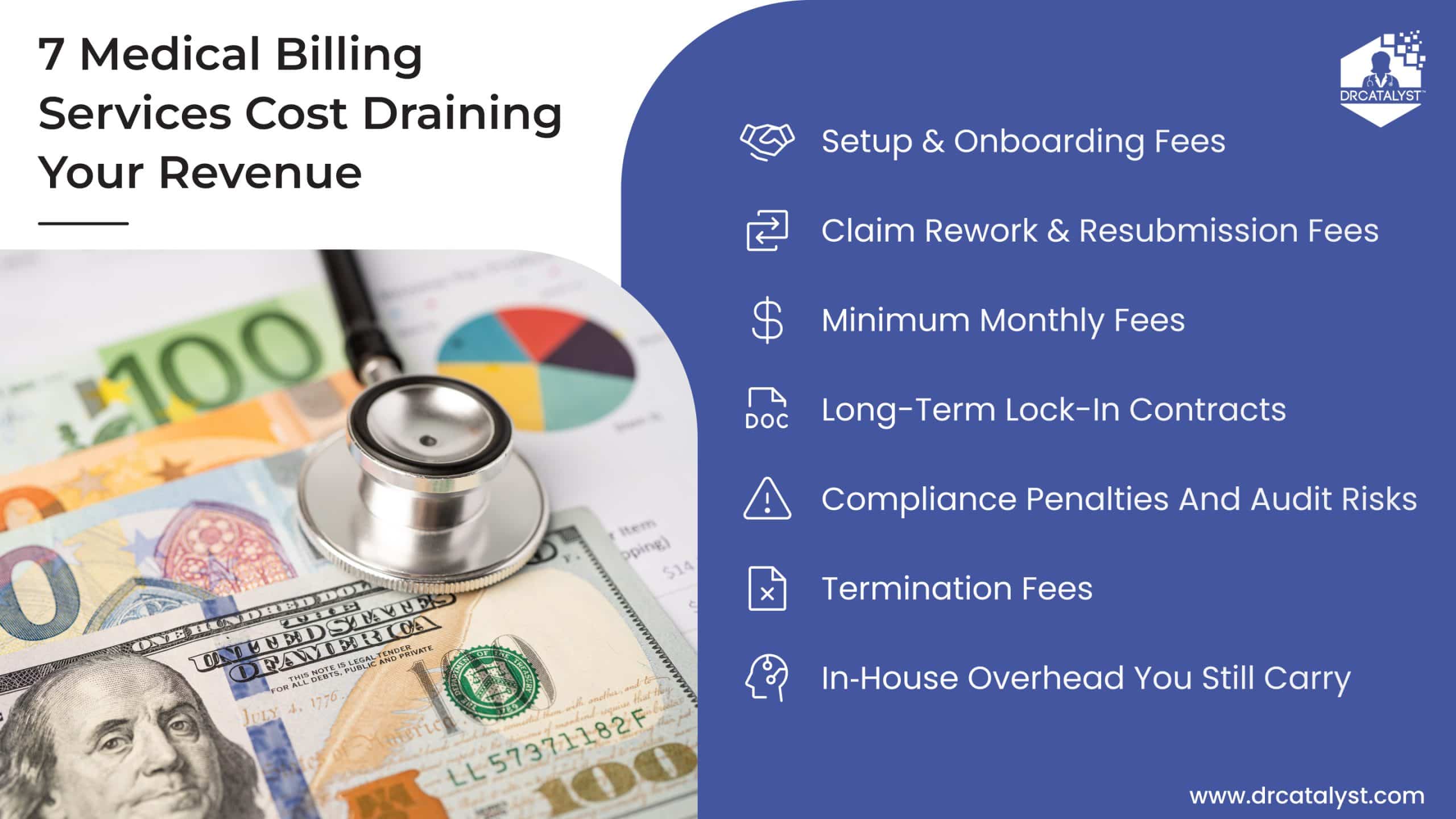
Hidden Costs to Watch Out for in Medical Billing Services
It is beneficial to be aware of how much medical billing services cost. Many times, these services have hidden costs involved that affect the revenue of your organization. We have picked some of the common hidden costs below and how they can be immediately avoided.
Setup & Onboarding FeesAre there initial costs for integration and data migration? A one‑time fee for onboarding, interface setup, and training are common scenario for many service providers. At DrCatalyst, we avoid these surprises with a clearly listed pricing structure. We want to ensure you do not experience any sudden, unexpected charges in your medical billing services journey with us.
Claim Rework & Resubmission FeesBe cautious if follow‑up on rejected claims, appeals, or patient balances is billed separately. This can dramatically increase the actual healthcare billing cost for practices with higher denial rates.
Termination FeesThis primarily accommodates the costs associated with ending a contract early. Unbeknownst to you, it can dramatically increase pricing when the quality is poor, and you wish to terminate the contract early.
Minimum Monthly FeesDoes the contract have a floor, even if collections dip? Some contracts include minimum claim volumes or revenue targets. When your practice is seasonal or still growing, you could pay more than the real average cost for the medical billing services you use.
Long-term Lock-in ContractsMulti‑year agreements limit your ability to pivot if service quality drops or your needs change.
Compliance PenaltiesAudit risks are significant concerns for healthcare practices. The ongoing training for HIPAA, billing regulations, and payer policy changes should be included, but it might be charged separately.
In‑house overhead you still carryEven after outsourcing, you may still be paying internal staff for tasks like front‑end eligibility, charge entry, or patient calls. These costs should be factored into the overall cost of “how much does a medical billing service cost?”
A low upfront price doesn’t always translate to lower total cost. This is especially true when revenue leakage and delayed reimbursements are factored in.
Contact us today to save your revenue leaks!
Why DrCatalyst is the Value-driven Choice?
At DrCatalyst, we believe in transparent pricing that reflects our commitment to your mission. We don’t just provide a service; we provide an extension of your team. When you hire medical RCM experts, designated billers or certified coders through our dedicated remote model, you gain access to specialists trained in your workflows. These remote assistants are trained in your protocols, work in your specialty, and EHR. This helps reduce your A/R days without the overhead of in-house staff. Instead of managing rising in-house costs, practices gain predictable billing expenses and measurable financial outcomes.
As a leading medical billing services provider, DrCatalyst handles-
End-to-end Billing ManagementFrom charge entry to payment posting, we handle and supervise every step of the billing process with accuracy and efficiency.
Example: When a multi-provider clinic completes a patient visit, DrCatalyst takes over immediately. Our remote team reviews documentation, validates charges, and submits clean claims within 24 hours. Your designated team of assistants tracks each claim through payer responses, follows up on rejections, posts payments accurately, and reconciles EOBs to ensure nothing is missed. If a denial arises, we correct and resubmit proactively before revenue is delayed. The end result is faster reimbursements, fewer denials, and complete visibility from first charge to final payment.Dedicated Virtual Medical BillersThe claims are often queued up in common outsourced services. DrCatalyst has a different approach with dedicated virtual billers. Our remote medical billers work exclusively with your practice. They are trained in your workflows, comfortable working with your providers, and familiar with common billing scenarios. Your designated team is not working in isolation. The billing team takes accountability and makes multiple touchpoints with you throughout the service. The end result of a shared expertise is to bring success to your revenue cycle management cohesively
Proactive Denial ManagementOur team doesn’t just appeal denials. We analyze the reasons and patterns behind these denials. As the next step, we implement preventive measures to reduce future denials to expedite your revenue.
Eligibility VerificationVerifying insurance coverage before services are rendered prevents costly claim denials and awkward patient conversations about unexpected bills.
Prior Authorization ServiceWe understand complex payer requirements for prior authorizations. It is critical for maintaining convenient treatments and avoiding reimbursement surprises. Our proactive Prior Authorization Service navigates complex payer requirements to ensure convenient treatments and eliminate reimbursement surprises. We provide end-to-end processing and meticulous tracking for all authorizations, integrated with comprehensive fax management and secured sending of medical records. This helps to meet strict documentation standards. We combine this with our dedicated credentialing services and payer contract renegotiation expertise, to stabilize your revenue stream. Our certified coders ensure initial coding reviews to validate E/M levels and provide actionable feedback for provider improvement.
Comprehensive ReportingReal-time access to customized dashboards and detailed reports that provide visibility into your practice’s financial performance.
Compliance AssuranceStay up to date with ever-changing regulations, coding updates, and payer requirements. Our remote assistants manage compliance. The complexities of eligibility, coding, aggressive denial management, and RCM services are addressed to balance your workload. We understand that cost is only valuable when paired with performance and scalability.
Need to scale your clinical team too? Explore our Remote Medical Staffing Services
Benefits of Our Virtual Staffing Services:
Cost Savings with Qualitative ServiceOur virtual medical billers provide premium services as compared to the hefty cost of hiring in-house staff. You avoid expenses like salaries, benefits, office space, training, and turnover while still receiving dedicated, accountable services.
Scalability and FlexibilityWe are aware that any practice does not have a linear graph in terms of growth or seasonal fluctuations. As a result, we ensure that your virtual team scales with you in times of need. If you need additional support during high-volume months, it is the RCM team’s responsibility to grow to cover all billing tasks without any hiring headache for you.
Designated AssistanceOur medical billers specialize in various practice types and specialties, from primary care to complex specialties, and from surgeries to orthopaedics. At DrCatalyst, we’ve a built in model to provide you expert assistance. We understand your protocols, take accountability to deliver you a 3+ levels of supervision with proactive communication in your billing services.
Integrated TechnologyYour virtual team integrates efficiently with your practice management and EHR systems. They work in your EHR/PMS as if they were sitting in your office without any significant technology transition. Your virtual team communicates productivity reports with you maintaining complete transparency.
Reduced Administrative BurdenPractice managers and physicians can focus on patient care rather than billing issues, staff management, and financial troubleshooting. We handle the complexity while keeping you informed.
Business ContinuityStaff illnesses, vacations, or turnover don’t disrupt your billing operations because we maintain backup coverage and knowledge transfer across team members.
Want to know exactly how much a medical billing service costs for your specific practice? Schedule a free consultation with DrCatalyst today.
Must-Ask Questions for Assessing the Medical Billing Services Cost
Before committing to any medical billing service, you should ask these critical questions:
About Pricing:
What services are included and excluded in the percentage or monthly fee?
Are there any additional fees for eligibility verification, prior authorizations, patient statements, or denial appeals services?
How do you handle low-volume months or seasonal variations?
Are there any early termination penalties?
About Services:
How quickly do you submit claims after receiving documentation?
Do you work the legacy AR?
What are time requirements for specific tasks to be completed like claims submission or payment posting?
How do they handle claim denials?
What is their frequency and type of reporting?
Do you offer eligibility verification and prior authorization support?
How do you handle patient billing and collections?
About Expertise:
Do you have any experience with the named specialty?
What EHR/practice management systems do you work with?
How do you stay current on coding changes and payer requirements?
What training does your billing staff receive?
Can you provide references from similar practices?
About Performance:
What key performance indicators do you track?
What average collection rates do your clients achieve?
How quickly do you turn around denied claims?
What is your average number of days in accounts receivable?
Investing in Healthcare Practice’s Financial Health
The detailed planning to estimate the costs of your medical billing services is a strategic exercise. The end goal of any healthcare organization should not be to find the cheapest option. Your service provider should be the most valuable solution in helping you reduce administrative burden, accelerate cash flow, and provide peace of mind. By understanding the factors, average costs, and potential pitfalls, you can make an informed decision that supports both your bottom line and your commitment to patient care.
Choosing the right medical billing company is an investment in your practice’s future. As you evaluate vendors, consider DrCatalyst. As a proven extension of your team, we’re focused on your long-term stability and success.
Ready to reduce billing costs and improve revenue?