Introduction
Medical billing is the financial backbone of every healthcare practice. Providing quality patient care remains your top priority. What keeps the doors open depends on accurate claims submission and on-time payment collection with minimal denials. That’s where a medical billing company steps in.
But here’s the challenge: the U.S. healthcare industry is changing rapidly, and so are billing rules. With higher claim denial rates, shifting payer requirements, and the demand for faster reimbursements, choosing the right medical billing partner in 2026 is more critical than ever.
The global shift toward outsourcing is accelerating this need. The medical billing outsourcing market has surged from $2.17 billion in 2021 to $13.56 billion in 2022. It is projected to reach $20.98 billion by 2026 ( GlobeNewswire ). This massive growth reflects exactly what healthcare practices are experiencing. Amid higher administrative burdens, staffing shortages, and complex payer rules, practices need to remain profitable.
In this guide, we’ll break down what a medical billing company does, why your choice matters, and how you can confidently select DrCatalyst as the best medical billing company for your practice.
What is a Medical Billing Company?
A medical billing company is a professional service provider that manages the entire billing cycle for healthcare practices. Instead of handling claims and collections in-house, practices outsource these tasks to specialised agents.
Here’s what a comprehensive medical billing company typically does:
- Prepare and submit claims to insurance providers.
- Handle coding (ICD-10, CPT, HCPCS) to ensure accuracy.
- Track claims and follow up on unpaid or denied submissions.
- Manage patient billing for co-pays, deductibles, and balances.
- Provide reports showing revenue, collections, and denial trends.
In short, they’re not just paperwork handlers; they’re the middle link between your services and your revenue.
What Medical Billing Companies Don’t Do (But you might expect them to)
Most billing companies don’t:
- Negotiate payer contracts
- Audit charts for documentation improvement
- Track quality metrics
- Work old/aged A/R from before their contract start
- Handle patient scheduling or intake accuracy
- Support multi-specialty complexities
But these gaps often lead to lost revenue, compliance issues, and unnecessary administrative burden inside clinics.
Why is choosing the right Medical Billing Partner important?
Not every medical billing company delivers the same level of expertise. The outsourced medical billing company you choose directly affects your practice’s financial health and daily operations.
Here’s what the right medical billing partner brings to your practice:
- Revenue:
Your revenue cycle is only as strong as the partner managing it. A skilled billing company reduces denials, speeds up reimbursements, works aged A/R, and improves your net cash flow position.
- Communication & Support:
Consistent, transparent communication ensures you always know the status of claims, denials, and collections. A reliable billing company acts like an extension of your in-house team, not an outsourced vendor.
- Certified Coders & Coding Accuracy:
Coding rules change every year. Incorrect or outdated codes lead directly to denials and underpayments. A strong billing partner provides certified coders trained in current ICD-10, CPT, and HCPCS guidelines, ensuring accurate documentation and maximizing reimbursement.
- Compliance & Data Security:
Your partner must protect sensitive patient data, maintain HIPAA compliance, and establish secure workflows across all RCM functions.
- Patient Satisfaction:
Clear, accurate patient billing reduces confusion and frustration. A strong billing company benefits patients with timely, understandable statements, helping enhance their overall experience with your practice.
Think of it this way- The wrong billing company can cost you thousands in lost revenue. The right one becomes a true medical billing partner who grows with your practice and improves your net cash flow position.
Top 10 Tips to choose the right Medical Billing Company in 2026
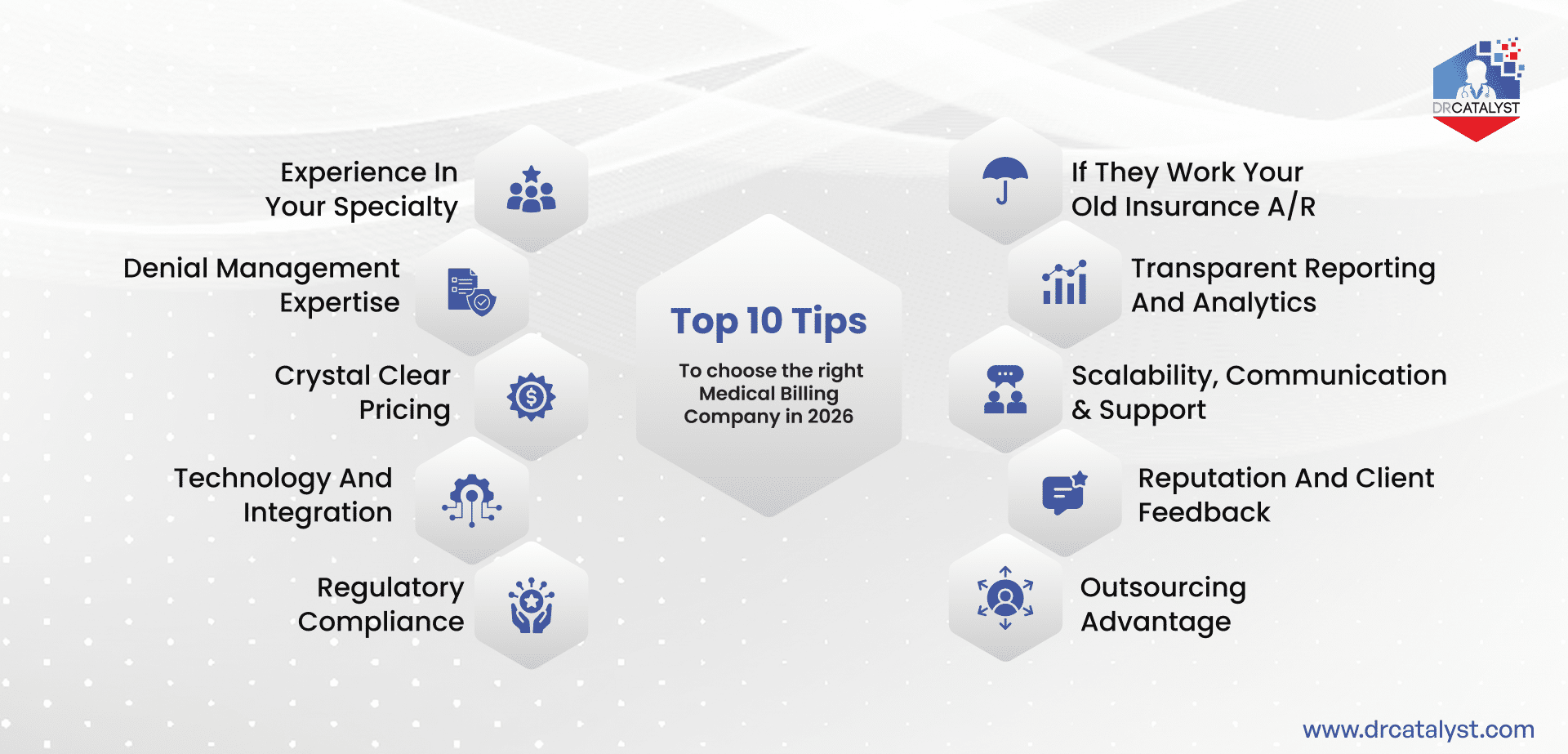
Here’s a checklist of what to look for before signing a contract:
1. Experience in your Specialty
Different specialties have different billing needs and quirks. Choosing a partner who understands the nuances of your specialty can make or break your revenue cycle. Whether you’re an Allergy/Immunology, Behavioral Health, or FQHC/Community Health practice, your billing rules, codes, modifiers, and denial patterns are unique. Always ask for references or proven experience in your specialty.
2. Denial Management Expertise
One of the biggest roadblocks is that a billing company pushes denials back to your clinic to ‘finish’ them. A true billing partner should take full responsibility for denial management, including correcting, appealing, and promptly resubmitting denials. It effectively communicates denial trends and patterns, enabling long-term prevention. You should always ask directly: ‘Who works the denials, you or our in-house team?’ The answer will tell you everything.
3. Crystal Clear Pricing
Transparent pricing isn’t just about knowing the invoiced percentage. It’s understanding what’s actually included in that invoice. Some competitors promote unrealistically low rates (e.g., 2–3%) that apply only to high-volume practices. Otherwise, they exclude critical services such as denial management, credentialing follow-up, and patient calls. A billing partner should have their pricing clearly listed upfront and reflect the real work, not misleading teaser rates.
4. Technology and Integration
It’s not just whether a company uses ‘advanced billing software’ but whether they work inside your existing EHR and billing system. Many medical billing companies require switching systems, or they’ll force you to use their proprietary billing system. This switch disrupts workflows and creates new problems. Choose a partner who adapts to your tech and integrates with your EHR/EMR or provides a smooth transition.
5. Regulatory Compliance
Compliance in medical billing extends far beyond HIPAA. A trusted billing partner must follow federal, state, and payer-specific regulations. These compliances would include CMS and OIG guidelines, Medicare and Medicaid billing rules, and annual updates to ICD-10, CPT, and HCPCS codes. Medical billing compliance also requires maintaining accurate documentation that meets medical-necessity standards and withstands RAC, MAC, and commercial payer audits.
Choosing a partner who prioritizes complete billing and coding compliance protects your practice from penalties, reduces denials, and keeps your revenue cycle audit-ready and financially secure.
Read More: October 2025 – Automatic Downcoding Threatens Independent Physician Practices
6. Will They Work Your Old Insurance A/R?
Before signing, ask whether the billing company will work your existing unpaid A/R or only handle new claims going forward. Many companies ignore historical claims, leaving you with thousands of dollars in uncollected revenue. A strong partner will help recover both old and new balances.
7. Transparent Reporting and Analytics
Beyond reports, ask whether your billing partner acts as a true billing consultant. Your partner should guide you on coding updates, changes in payer rules, denied claim trends, and annual CPT/HCPCS code revisions. The adherence to these updates ensures your clinic stays compliant and profitable.
8. Scalability, Communication & Support
As your practice grows, your billing partner must scale with you. Your billing company must be able to handle higher claim volumes without sacrificing accuracy or timeliness. A reliable billing partner stays accessible, answers questions quickly, and functions like a team member. Together, scalability and strong communication ensure smooth operations, long-term collaboration, and uninterrupted revenue performance.
9. Reputation and Client Feedback
Check online reviews, testimonials, and case studies. A reputable medical billing company will be transparent about its client success stories.
10. Outsourcing Advantage
When comparing in-house vs. outsourced billing, don’t just compare salaries. Include the real cost of:
- Staff benefits
- Office space and equipment
- Training time
- Productivity losses
- Turnover
- Unworked aging A/R
A qualified third-party medical billing partner offers an entire team of coders, billers, denial experts, and RCM consultants for a fraction of in-house cost. Before choosing, request a cost analysis comparing your current in-house billing expenses vs. a third-party billing team to see the actual financial impact.
Why DrCatalyst is your Best Medical Billing Partner?
At DrCatalyst, we’ve been helping practices take control of their revenue for over 16 years. Here’s how our services enhance your medical billing process:
New Patient Coordinator Service
- Intake Accuracy:
We enter patient demographics and insurance into your EHR, reducing data errors that lead to denials.
- Chart Readiness:
We collect required medical records and summarize the patient’s history to prepare the chart before the doctor’s visit.
- Scheduling & Follow-up:
We handle patient communication, scheduling, and sending reminders.
Provider Credentialing & Contract Negotiation Services
The essential process of enrolling healthcare providers with insurance payers (Medicare, Medicaid, private insurers) to legally bill and receive payment.
- We manage the entire intricate credentialing lifecycle from initial application submission and follow-up to ongoing re-credentialing and payer roster maintenance.
- Our credentialing assistants ensure you can see patients and get paid without delays or compliance issues.
Revenue Cycle Management (RCM) Solution
Our comprehensive Revenue Cycle Management service covers every touchpoint from patient registration to final payment.
Front-end RCM:
- Insurance eligibility verification
- Benefit investigation and pre-authorization
- Patient financial counseling and estimates
- Registration accuracy audits
Mid-Cycle RCM:
- Professional medical coding (certified CPCs/CRCs)
- Charge capture and entry
- Claim scrubbing before submission
- Electronic claim submission and tracking
Back-End RCM:
- Payment posting and reconciliation
- Denial management and appeals
- Insurance AR follow-up and collections
- Patient billing and payment plans
- Monthly financial reporting and analytics
- 1400+ virtual medical assistants and billers.
- Proven track record with 500+ happy clients across specialties.
- Dedicated teams for denial management, coding, and patient billing.
- Medical Billing Solutions designed to cut overhead and boost collections.
- Secure and HIPAA-compliant
Here’s why many providers choose DrCatalyst as their trusted Medical Billing partner:
Conclusion
Choosing the right medical billing company in 2026 is a financial and strategic decision. A reliable partner ensures your practice stays profitable, patients are billed correctly, and compliance is never at risk.
As claim denials rise and administrative costs increase, partnering with an experienced billing team is essential. Whether you’re a small clinic or a multi-specialty hospital, the right choice can transform your revenue and free up valuable time from administrative backlog.
If you’re ready to make the shift, DrCatalyst is here to help. Explore our full range of medical billing solutions today.