In October 2025, major insurers Cigna and Aetna rolled out new automatic downcoding policies for Evaluation and Management (E/M) services. This has created immediate challenges for independent physician practices aiming to maintain compliant, profitable operations. These insurers have framed the move as a cost-containment and fraud-prevention effort. However, the effect on honest, independent practices is a tangible financial hit and more complex paperwork.
Understanding this threat is the first step to fighting back. Contact DrCatalyst today to learn about the impact of downcoding on your practice.
What’s New: ASIPP and Automatic E/M Downcoding
Aetna and Cigna frame downcoding changes as “fraud prevention” and “cost containment” efforts. The American Society of Interventional Pain Physicians (ASIPP) warns that Cigna and Aetna are relying on opaque algorithms and claims data. In absence of clinical documentation review, can downgrade E/M services. According to ASIPP, overcoding of E/M Level 4 and 5 visits accounts for only 0.13% of Medicare claims. It is far too insignificant to justify these drastic policy changes.
For instance, a Level 5 office visit (CPT 99215) is often automatically downcoded to a Level 4 (CPT 99214), and Level 4 visits are downcoded to Level 3.
This “deny first, pay later” approach presumes physicians are “upcoding” until proven innocent. For Cigna, AI-driven systems automatically downgrade submitted claims at the point of review, primarily impacting codes 99204, 99205, 99214, 99215, 99244, and 99245. Aetna focuses on post-payment audits. It reduces or claws back payment if retrospective documentation checks fail to support the initial code. In practice, the burden falls on honest physicians who must now appeal legitimate claims just to be paid correctly.
The Rising Administrative Burden on Providers
The financial loss from the downcoding is only part of the problem. These automatic downcoding policies create an unbearable administrative burden for providers. They face:
- Increased Appeals
Every downcoded claim requires staff time to track, prepare, and submit a formal appeal, often involving complex documentation packets.
- Coding Audits & Scrutiny
The payer policies place providers under constant compliance scrutiny.
- Claim Resubmissions
Practices must divert the billing team towards manually appealing for appropriate reimbursement, increasing their backlog.
Many small practices will eventually sell to hospitals or corporate health networks, accelerating the trend of consolidation in healthcare. Other independent practices might fail to manage the volume of appeals. They will reluctantly accept the financial loss which is an outcome the payers are counting on! This shift limits patient access to affordable, local care. It also erodes physician autonomy. Automatic downcoding isn’t just a billing issue. It’s a systemic pressure point designed to push smaller providers out of the market.
Fight Back Against Downcoding with DrCatalyst
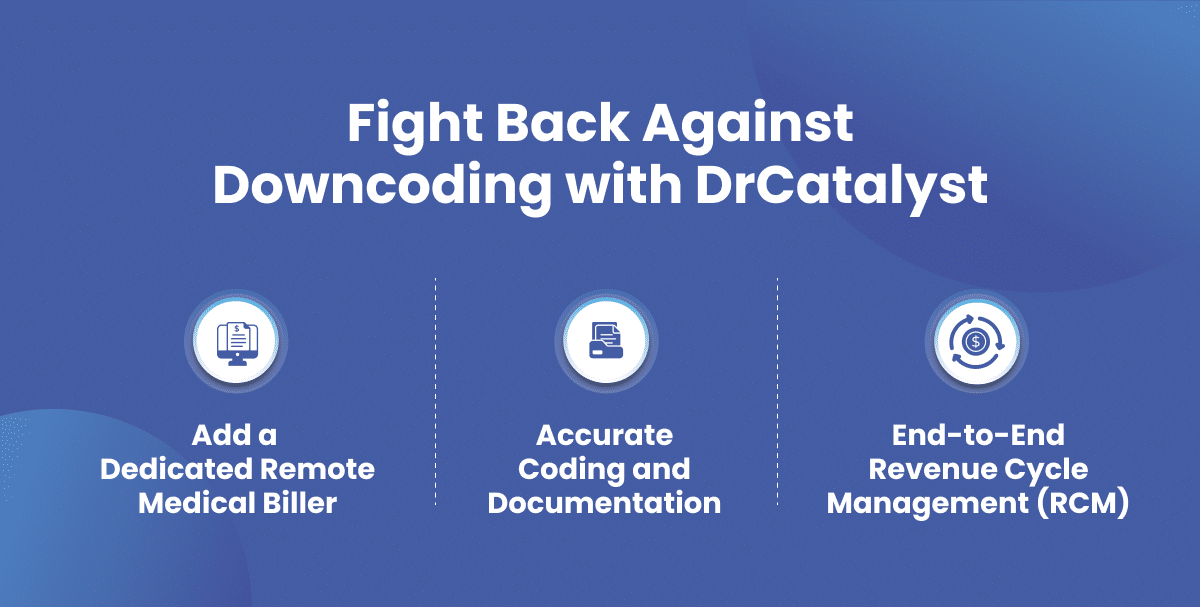
You don’t have to accept this new status quo. At DrCatalyst, we stand with independent practices from coding and billing to denial management and appeals. Our specialized remote teams are an extension of your practice. They’re equipped to handle the increased administrative load and protect your revenue. DrCatalyst’s remote coding, billing, and revenue cycle management teams deliver:
- Accurate Coding and Documentation
Our experienced medical coders follow payer-specific E/M guidelines to ensure every claim is correctly documented and justified. We proactively flag potential issues before submission to reduce denials and downcoding. This creates a stronger, defensible claim from the outset. Learn more about our robust Medical Coding Services.
- Add a Dedicated Remote Medical Biller
Our billing specialists identify downcoded claims, manage the entire appeals process, and resubmit claims with the necessary documentation to fight for the reimbursement you deserve. Discover more about our Medical Billing Solutions.
- End-to-End Revenue Cycle Management (RCM)
With our full-scale RCM services, we build resilience into your entire financial workflow. From eligibility verification to final payment, our team ensures your entire revenue cycle runs smoothly. We strive to minimize claim delays, denials, and administrative overhead. Protect your bottom line with our complete Revenue Cycle Management.
Conclusion
Aetna and Cigna’s automatic downcoding policies mark a critical turning point for independent healthcare providers. They need to fight unfair payment reductions and preserve every dollar they earn. Let DrCatalyst help you secure your revenue, protect your compliance, and reduce administrative strain in 2025 and beyond.
Stay tuned for a follow up article on: How to Strengthen Your Appeals and Prevent Downcoding Under Cigna and Aetna’s New Automatic Downcoding Policies?