Privacy Notice: Use of Google Analytics
DrCatalyst uses Google Analytics to understand how users interact with our website, helping us improve your experience. Data collected (e.g., pages visited, time spent, location) is anonymized and stored securely, with no personal information shared. Learn more via Google's Privacy Policy. To opt out, adjust your browser settings or use the Google Analytics Opt-out Add-on. By clicking “Accept”, you consent to this data collection.
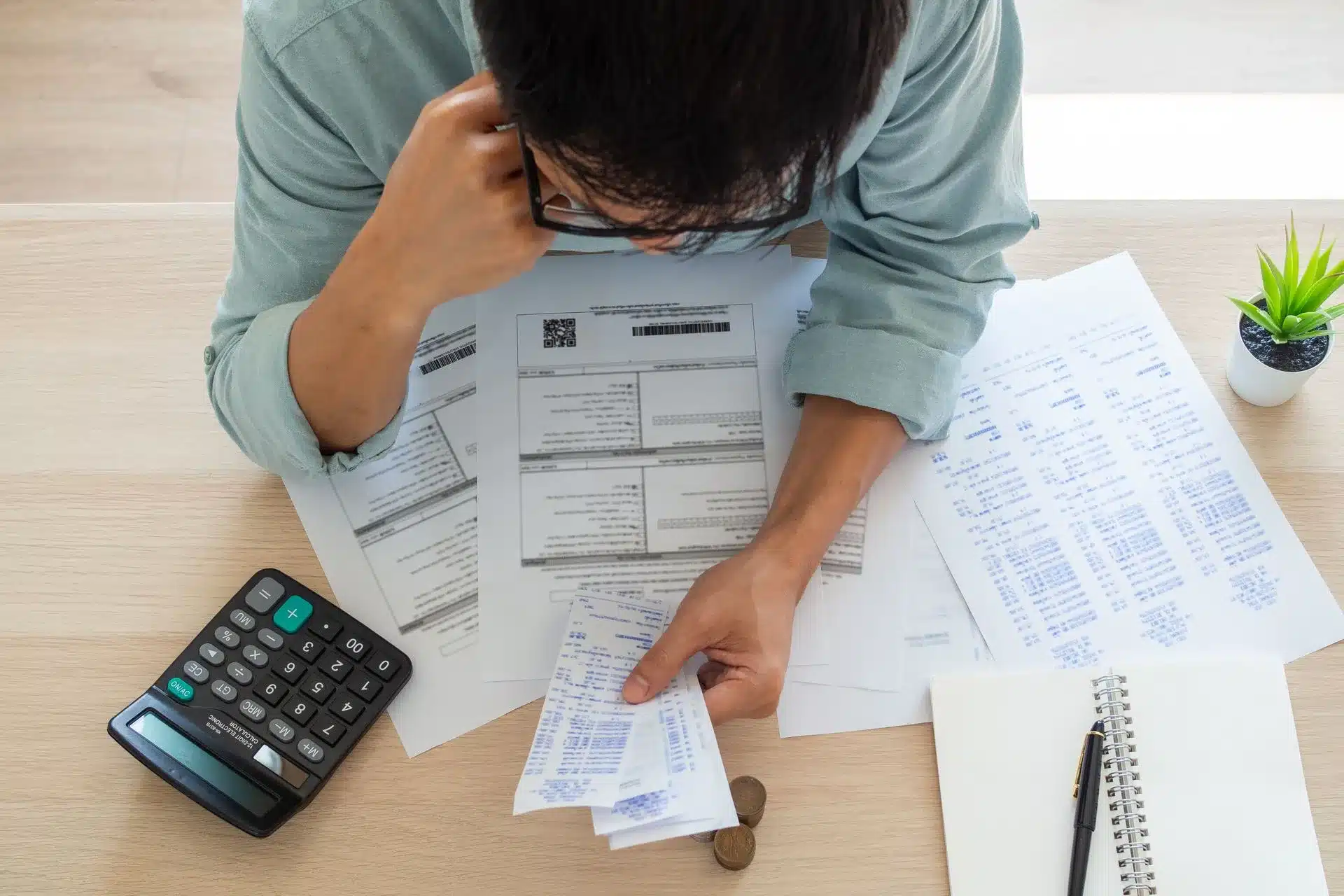
 Navigating the intricate world of immunotherapy billing can be as challenging as administering the treatment itself, especially for healthcare providers specializing in allergy immunotherapy.
Navigating the intricate world of immunotherapy billing can be as challenging as administering the treatment itself, especially for healthcare providers specializing in allergy immunotherapy.